The implementation of healthcare integration benefit the industry in many forms, including cutting operating costs, and offering consistent and quality care services. The demanding task concerning integration requires overcoming some integration challenges.
What is Healthcare Integration?
Healthcare integration or, more precisely, health data integration and utilization, is the process of aggregating the health data from different sources for further collaborative use to improve clinical decision making and patient self-management support. According to studies, integrated healthcare is likely to reduce cost and improve outcomes.
However, health businesses often struggle with aggregating health data (both of structured data and unstructured data) from initially unconnected healthcare data sources such as EHR systems, hospital information systems, medical imaging systems, wearable devices, health applications and so on, as well as with further utilization of integrated data.
To overcome the issue, integrated health information platforms are implemented. They have three critical components: the main data integration server, healthcare integration tools connected to required data sources, and dashboards/reports for end users.
Data extraction (E), transformation (T) and loading (L) into a unified database - this is how a typical simplified ETL/ELT-based health data integration process may look like.
To make it real one needs:
- use a unified database to put data in,
- use data extraction scripts for each data source,
- use data transform scripts to modify the extracted data to required format to fit the structure of the single database,
- use data loading scripts to import the transformed data into the database.
After the data is integrated, the task is the utilization of integrated data that is realized through different user interfaces including dashboards and reports.
Healthcare Integration Tools
Healthcare data integration tools are divided into custom and off-the-shelf ones.
The advantage of custom data integration tools is your full control over functionality, for example because of data security requirements. It’s an option if tools available in the market are unable to meet all your needs.
Among the cons of commercial data integration tools there are may be:
- complex pricing models: customers find cost planning difficult in determining scenarios and budget projections;
- high licensing costs for particular tools and a longer time to achieve ROI objectives;
- hard-to-understand documentation;
- limited integration capability with other solutions.
In its turn the pros of ready-to-use data integration solutions are their capabilities of immediate implementation. However, there are three “ifs” involved:
- if the tool is right for you,
- if you don’t have to buy the entire platform,
- and if there are no problems with finding skilled implementers.
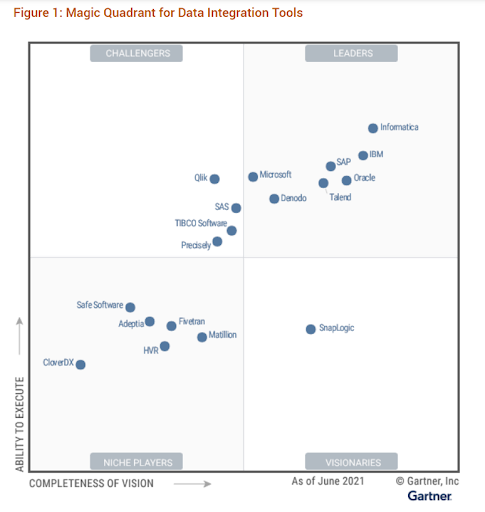
Gartner’s Magic Quadrant for Data Integration Tools (2021) lists 18 vendors who provide off-the-shelf data integration tools that can be purchased independently from broader data management platforms. They excluded vendors that only provide support for open-source platforms/frameworks or development platforms, which need to be heavily engineered/customized for specific data integration tasks/use cases and/or are specific to a single data integration/data delivery style (such as stream data integration only).
The key issue is how to select the right tool in support of the health data management solutions in your healthcare organization.
To narrow down the list you need to understand what types of data integration techniques you need to use, and, accordingly, which data integration tool provides this functionality.
Data integration techniques:
- bulk/batch data processing (processing of a large volume of data all at once not in real-time through ETL or ELT procedures; it can be used, for example, for patient management or verifying patient eligibility);
- data replication (copying data and storing them at different physical locations through change data capture (CDC) procedures);
- data virtualization (access, and manage data in real time when requesting via middleware without replicating it in a physical repository);
- streaming data integration (major use case is real-time analytics for sensor data);
- data synchronization (synchronizing data between two or more sources and target location and updating changes automatically between them).
- data orchestration (process of coordinating the execution of different data processing tasks).
Gartner suggests that tools from 18 vendors meet all criteria, and tools from additional 10 vendors (Honorable Mentions) almost meet them.
Their matrix consists of Liders (including Microsoft, and Oracle), Challengers (including Qlik), Niche players and Visionaries. As to Honorable Mentions this category includes Amazon Web Services and Google Cloud Platform.
For companies which are interested in evaluating and procuring tools that specialized ONLY in one data delivery style (for example, data replication, data ingestion, API integration, self-service data preparation or data virtualization) or support one use case (such as cloud data ingestion and migration), one data type (such as IoT data integration) or one scenario (such as location intelligence through geospatial data integration focus) Gartner recommends confidently start with the vendors in the Niche Players (including Adeptia Connect, CloverDX Data Management Platform, and Safe Software).
Additional criteria that may help you find the best data integration tool:
- support integrating data across different cloud infrastructures and synchronize it with on-premises data sources and targets;
- don’t necessitate the movement and persistence of data into a specific vendor repository or cloud ecosystem;
- allow to integrate data across different data stores, applications or multicloud/hybrid environments to avoid potential vendor lock-in challenges and data silos;
- allow data engineers to build, manage, operationalize and even retire data pipelines in an agile and trusted manner, as well as run their pipelines in various execution environments;
- allow optimizing code and pipeline execution through pushdowns, containerizations and serverless execution.
EHR Integration as the Core Component of Healthcare Integration
EHR can be connected with dozens of essential medical systems to enable easy data exchange, eliminating data entry repetition, and saving both physicians and the IT department hours. If necessary, data from legacy systems can be converted into EHR along with the integration process, which may include encounters, transcription data, radiology data or vaccination information.
Different organizations have different needs, but below are some of possible integrations: medical device EHR integration, telehealth EHR Integration, integration EHR and billing, EMR lab integration, and PDMP EHR integration.
Medical Device EHR integration
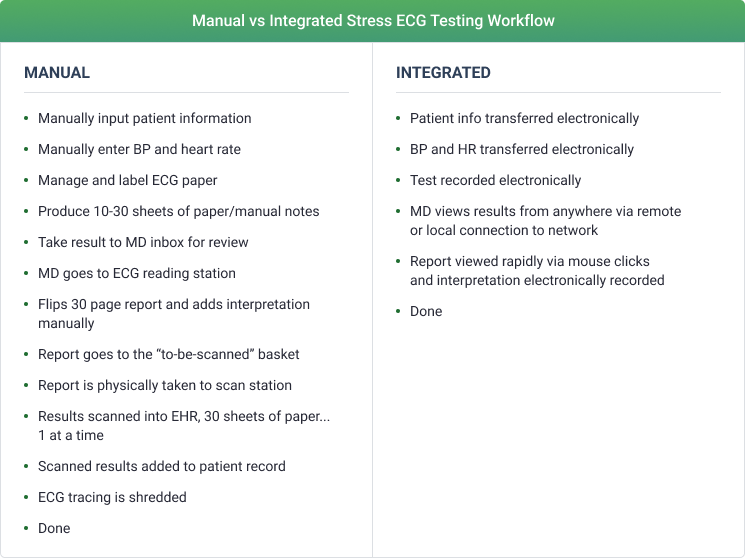
The quality of clinical decisions is directly related to immediate availability of the most current data to physicians.
Often, nurses have to transcribe and chart manually vital signs like respiratory rate, oxygen saturations, temperature, systolic blood pressure, pulse rate, level of consciousness and so on. The information is not available immediately and it’s associated with the risk of inaccurate and incomplete patient ID, transcription errors or lost readings.
Actually, it’s better to have a list of patients up on the screen, so that one can go around and individually look at the triggers’ alerts if measurements are outside normal ranges.
The workflow automation in this case may look as the following:
- Patient's barcoded wristbands send patient vital signs to the medical device integration middleware;
- The middleware is configured to get information from the hospital devices using different protocols and to communicate with the EMR using HL7 messages; It understands patient's identification numbers and can update the right patient records in the EMR system;
- Such middleware supports sending device data results to EMRs in both PDF report form and HL7 discrete data (all versions of HL7® 2.x, 3.x, extended and non-standards compliant versions, including the HL7 FHIR® standard). In addition, there is also built-in support for DICOM, NCPDP, CCD/CDA, X12 EDI and more.
Remote patient monitoring (RPM) is a valuable tool in conjunction with telemedicine.
Telehealth EHR Integration
Not all video platforms are designed for telehealth from neither a HIPAA nor interface standpoint. Especially if one needs to download a separate application.
Actually, it’s better to embed a telehealth solution within the EHR system to make a doctor’s workflow similar to checking in a patient at the office. Such integration eliminates multiple clicks to switch between documentation and video screens. The patient can also have easy access to telehealth via the patient portal and can schedule a future appointment by staying on the video chat after completing the visit.
With the camera and the EHR on the same screen, doctors are able to look at the EHR while doing documentation and then move their eyes a little to look into the camera and talk to the patient. Additional options for EHR medical documentation during telehealth visits include using speech recognition solution for dictation, or using a scribe during the appointment.
The added bonus is the ability to have several users in the visit at one time, for example, a nurse can enter and leave the visit without disrupting the visit for other participants.
Telehealth solutions also allow providers to share screens with the patient while going over diagnostic results or providing patient education.
The provider can easily create a visit summary and send it to the patient with orders for diagnostic tests through the same interoperable interface.
Integrated EHR and Billing
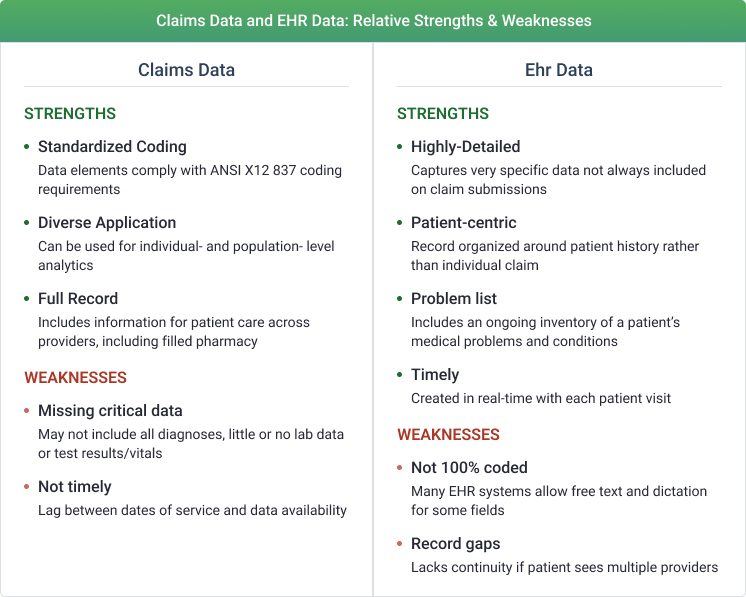
Often, EHR systems and the revenue cycle billing (RCB) systems are different software. So the billing team spends a considerable amount of time cross checking patient data and filling up the claim forms. Especially, when clinical information is needed for proof, for example, that a particular condition was diagnosed before a therapy can be authorized.
Integrated EHR systems automatically pull the required data, including coding, from the patient forms and medical records to the claim form reducing the chances of mistakes. Such integration typically requires HL7 interfaces to exchange demographics, appointments, encounters, and charges.
Built-in alerts and reminders help ensure that providers record all relevant procedure codes, diagnosis codes, and supporting documentation in each patient’s medical record. This approach reduces the risk that payers will deny claims.
EMR Lab Integration
Often, some components of the lab test result (as a separate HL7 ORU RO1 result message) are sent to a provider clinic EMR hours before others, even when they are part of one ordered test. Physicians are being overwhelmed with a seemingly endless stream of medical lab result alerts.
Actually, all medical lab results under one order should be sent together on a single result message to a provider.
The workflow automation in this case may look as the following:
- receive separate messages from the Lab system;
- organize the data in a database;
- aggregate multiple messages into one message, if they are associated with one order ID;
- send all combined messages to a provider clinic EMR on a specified schedule.
PDMP EHR Integration
To combat prescription drug abuse the prescription drug monitoring program (PDMP) is implemented as a statewide electronic database which collects data on controlled substances.
Often, doctors have to stop working with their EHR, log into the PDMP, put in all the patient information (enter username and password; navigate to a patient request; enter a patient’s first name, last name, and date of birth; determine a date range to search; select which states to query; click ‘search’....), wait for a return to come back in, and then look at it. That could take up to 10 minutes for each client.
Actually, it’s better to integrate the EHR or Pharmacy Management System with PDMP.
The workflow automation in this case may look as the following:
- The patient’s demographic information passes from the EHR to the state PDMP to execute the search automatically, for example, when the patient arrives for the appointment;
- The PDMP creates a risk factor for the patient, transfers the data back into the EHR system, and links it into the patient’s EHR to show the doctor more detailed information on the patient’s past prescribing history.
Healthcare Integration Challenges
Patients’ diagnoses, medications, and other key information should be accessible regardless of where they were documented. EHRs must be able to share data between different health systems especially when providers need to get information from previous visits. While the EHR system is the core component of modern healthcare, healthcare integration challenges often mean EHR interoperability challenges.
EHR Interoperability Challenges
Interoperability is the successful exchange of health information, when patients and clinicians have data when and where they need them. However, today there are some factors that prevent interoperability, including inadequate patient identity matching and low utilization of HL7 FHIR API. Using efficient data analysis and visualization tools, like run charts, can significantly contribute to the ongoing monitoring and enhancement of these processes.
Inadequate Patient Identity Matching
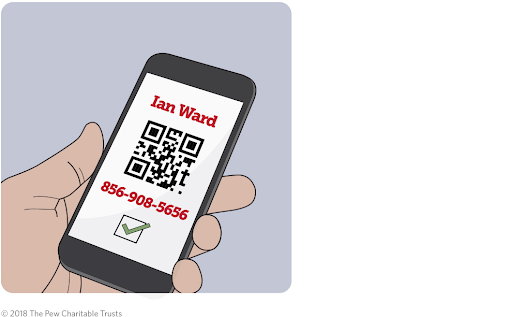
Patient identity matching is the possibility to successfully search each patient’s record in disparate systems and know that it refers to the same person.
The absence of this feature leads to safety problems, for example, if an allergy listed in one record is not documented in another system, individuals may get treatment that should be avoided. It also leads to costly repeat tests.
Another problem is false positive matches which could result in patients getting treated based on information of other patients, including incorrect diagnoses or unneeded medications.
Main factors to inadequate match rates:
- One system may contain addresses in a single field, while another - in several fields by separating street names from the city and state. It’s hard to impossible to match such data.
- Different systems match different persons as the same one due to the insufficient amount of data to compare, for example, the availability of different records with the name Maria Garcia and the same birthdate doesn’t mean that the records describe the same person - in some regions, certain names are extremely common.
- Different systems aren't capable of matching different records with one person due to the lack of information in one of the systems because the necessary data was not initially entered.
Despite the fact that currently there is no existing solution to achieve perfect match rates for all patients, several actions can be taken to better link records. Health care providers and technology vendors can embed phone number verification as well as some other solutions like the use of biometrics as the identifier. The use of smartphone applications with these features can help millions of patients, especially individuals with multiple chronic conditions and those who seek to be more involved and engaged in their care.
Low Utilization of HL7 FHIR API
API sends information back and forth between a user and a website or app. API-enabled apps focus on improving clinical workflows and advancing patient care to motivate patient and provider adoption.
APIs are a more cost-efficient route to EHR optimization for specific branches of medicine, for example, for pediatric use. Agencies continuously put out new policies and guidelines and their implementation in the EHR requires huge investment. APIs allow to create independent specialized software modules to extend EHR functionality, they are easier to develop, and test.
Regulations require use of the most recent version of Fast Healthcare Interoperability Resources (FHIR) standard (at date of publication) and the associated implementation guides, which were developed by Health Level Seven International (HL7).
FHIR allow providers to exchange only the information needed to inform care decisions - such as a list of medications or recent diagnosis, mitigating the need to exchange full clinical documents. For example, the Immunization FHIR includes only the patient, vaccine given, the administering practitioner, and some other data. When third-party developers request information like whether a patient received a particular vaccine, they receive only the requested data elements from the system.
API-based clinical decision support (CDS) tools can synthesize years of patient data in useful ways, transforming the health record from simply an information repository into an analytic technology. Embedded in the EHR such systems eliminate requirements to do extra steps like to manually launch an antibiotic recommendation app, input relevant data, and then return to the patient record to enter the suggested medication and dosage.
However, variation in FHIR implementation, differences in data vocabularies, and a lack of a standardized patient matching solution hold the API implementation back from reaching their full potential.
More companies like Amazon, Google, Microsoft, created fully managed FHIR cloud platforms for storing data in FHIR format, as well as securing Protected Health Information (PHI). These platforms allow developers to deploy FHIR services in the cloud, provide access control and audit, legacy data.
How Belitsoft Can Help
Our EMR integration company integrates healthcare solutions owned by our clients into healthcare organizations' EMR systems, creating lasting value for providers, patients, and administrators. We have experience managing successful client-facing integration projects, working in integration-focused roles, integrating external solutions via SMART on FHIR, and handling technical project management and solutions engineering at B2B healthcare software companies.
Rate this article
Our Clients' Feedback
































We have been working for over 10 years and they have become our long-term technology partner. Any software development, programming, or design needs we have had, Belitsoft company has always been able to handle this for us.
Founder from ZensAI (Microsoft)/ formerly Elearningforce