The AI medical coding market is a high-growth industry, with a CAGR of up to 14% over the next five years, according to various software market trend reports. This indicates growing interest in this niche among buyers (physician groups, health systems, billing and coding companies), investors, and medical technology startups.
What is AI Medical Coding Software?
AI medical coding products independently translate clinical information into billing and medical codes with up to 96% accuracy in coding predictions, without human intervention. This significantly reduce claims submission times and denial rates, especially during fluctuations in volume of documentation.
Human coders are only involved in resolving cases with low confidence scores, as defined by the software.
AI medical coding software is based on machine learning models that can make mistakes, which are identified during audits. However, the models can learn from corrected mistakes and prevent future errors. They can also be fine-tuned to follow updated coding guidelines.
At the technical level, this type of software uses NLP, deep learning, and LLMs to interpret clinical notes, including differentiating words based on context (contextualized embeddings) and capturing nuanced meanings of words (self-attention mechanisms).
The architectural approaches of such software may be based either on end-to-end deep learning models trained on large labeled datasets or on hybrid architectures involving rule-based systems.
Top-11 Medical Coding Software Startups
#1CorroHealth PULSE
- Funding: $376.4M
- Country: USA
The software uses computer-assisted coding (CAC), NLP, and knowledge-based AI. The NLP examines clinical semantics and concepts and assigns charges and codes according to predefined rules. It claims to provide 97% of coding accuracy. If the system does not meet the confidence limits, it sends the data to human coding experts for finalization.
The solution integrates with any EHR system. It supports both fee-for-service and value-based care coding.
PULSE automates the following procedures: assignment of charges, CPT and HCPC codes, diagnostic classifications, and E/M levels. It supports coding for urgent care, hospitals, clinics, physician practices, and radiology.
PULSE is developed in partnership with a US tech university.
#2 Fathom
- Funding: $61M
- Country: USA
The Fathom platform uses AI deep learning and LLMs to automate medical coding and perform audits. Fathoms codes for E/M, CPT/HCPCS, and ICD. The system works for primary care, ED, radiology, surgery, and other specialties.
The Fathom software handles around 90% of patient charts of healthcare organizations with a few thousand staff. The rest of the charts are transferred to human coders. It’s claimed that the algorithms examine best practices and improve accuracy with every next performance.
While performing audits, the platform also checks the accuracy of the coding and marks charts that may be denied. Those issues require fixing.
Banner Health, One Medical, UCI Health, Deaconess, Assembly, and other healthcare organizations use Fathom.
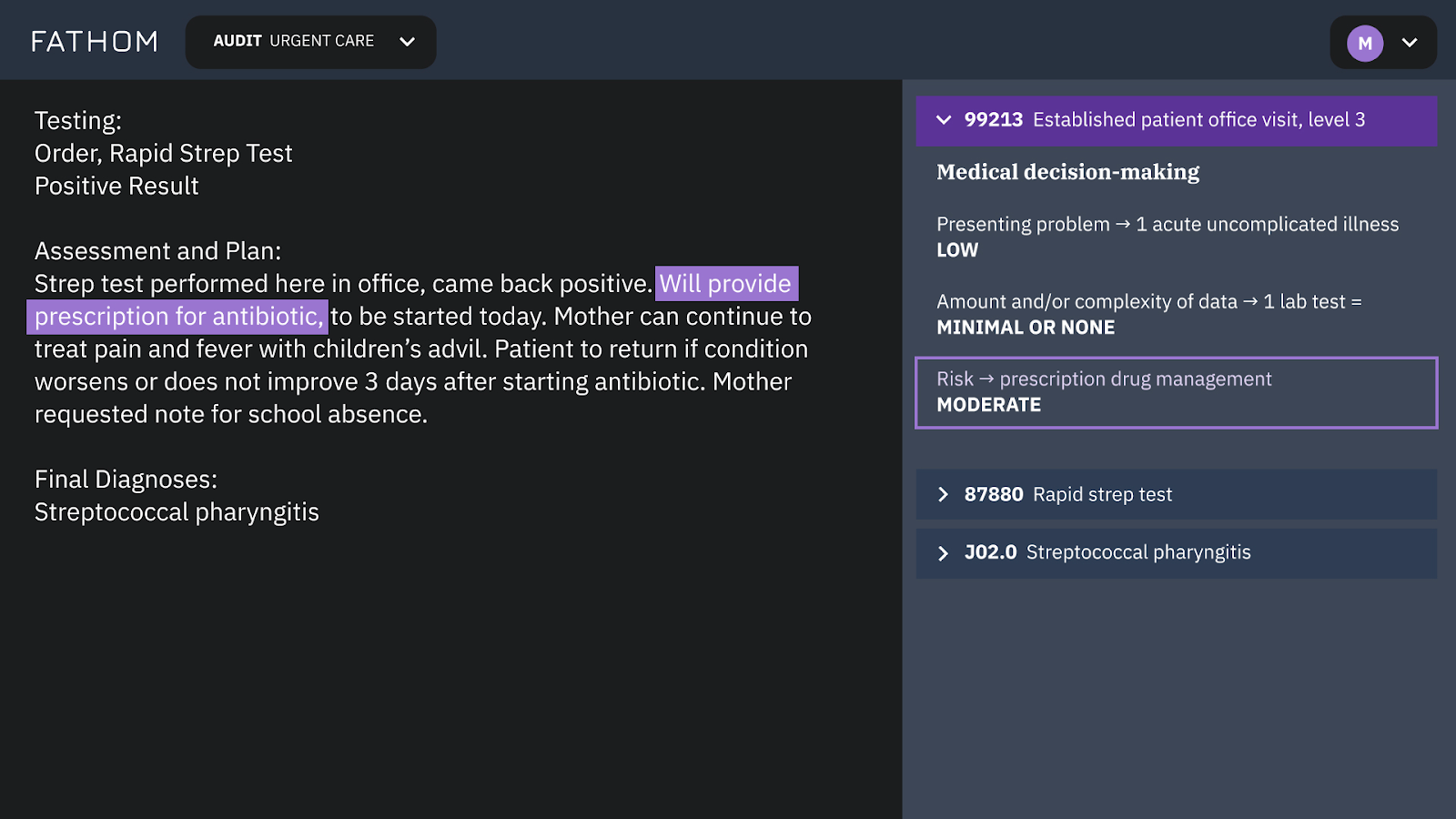 The system processes medical notes for patient visits to an urgent care facility and assigns medical codes
The system processes medical notes for patient visits to an urgent care facility and assigns medical codes#3 CodaMetrix
- Funding: $55M
- Country: USA
This is a cloud-based AI platform. It is used for medical coding in such specialties as radiology, pathology, evaluation and management, endoscopy, and surgery. The platform connects with an organization’s infrastructure.
CodaMetrix has the CMX Automate feature that uses AI, ML, and NLP.
The platform's embedded analytics help generate reports and examine trends in coding data.
The solution is compliant with HIPAA regulations and ICD-10, CPT, and HCPCS guidelines.
It’s claimed that the software brings 70% less denials than with manual coding.
Henry Ford Health, CU Medicine, Mount Sinai, UMass Memorial Health, Mass General Brigham, YaleMedicine, and other healthcare systems use CodaMetrix.
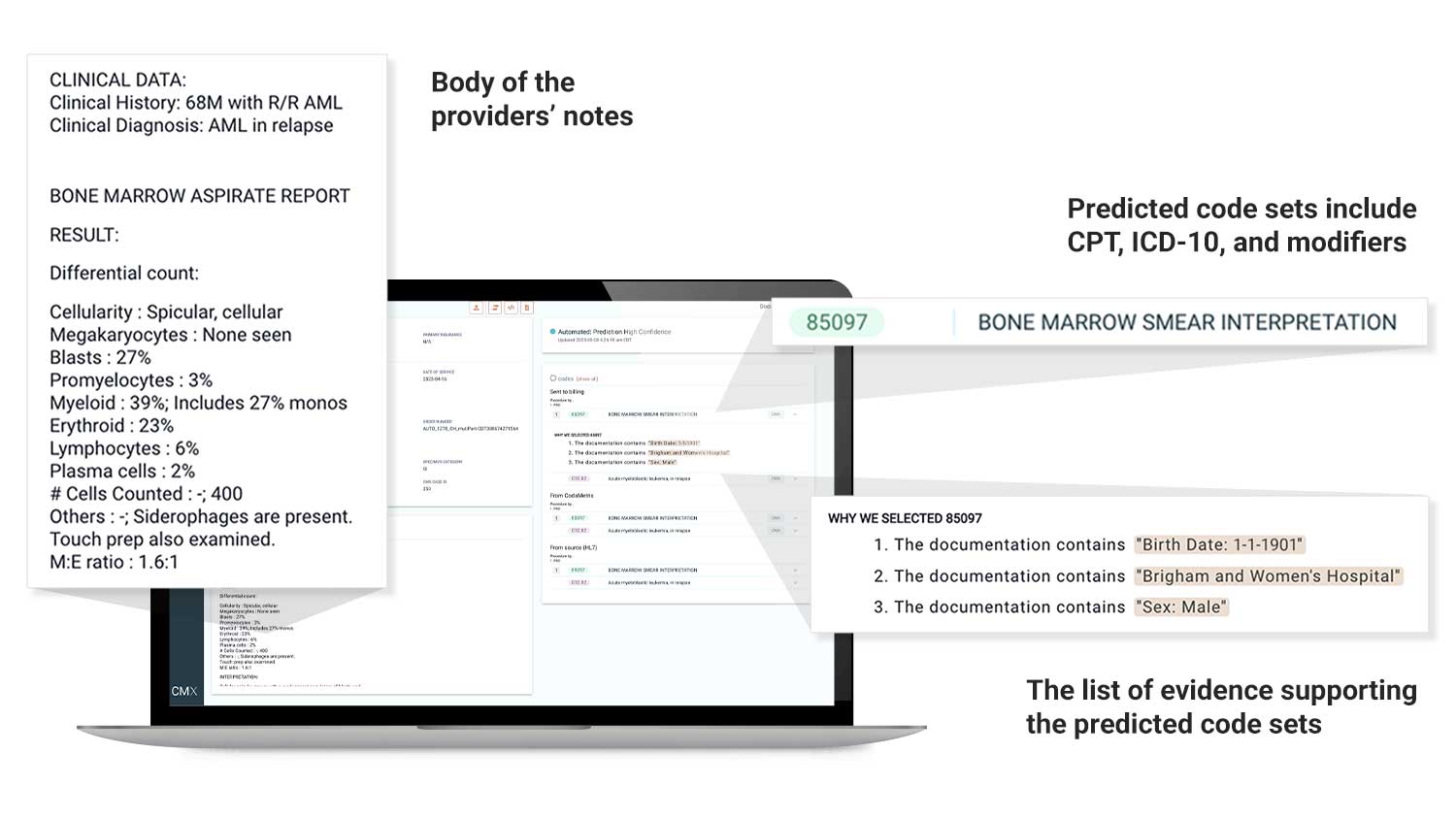 The CodaMetrix AI reads clinical notes, assignes, and justifies codes
The CodaMetrix AI reads clinical notes, assignes, and justifies codes#4 Nym
- Funding: $47.5M
- Country: USA
Nym applies its proper clinical language understanding (CLU) technology to “understand” and decipher the transcription of doctor-patient interactions and assign a relevant code (ICD-10 and CPT) to medical notes. It provides an explanation of the choice of codes in the form of audit trails. These trails become helpful in case of denials or compliance issues. If Nym fails to process a patient chart, it labels it for human coders.
Nym offers services for outpatient coding for both professional and facility charges, and inpatient coding for professional charges. The product supports six specialties of outpatient and inpatient care.
Nym’s engine seamlessly fits the existing environment. It sends medical records to billing without special validation from coders.
The software claims 95% accuracy and zero human intervention.
More than 150 healthcare facilities use Nym. Ochsner Health, Geisinger, Prisma Health, The University Hospital of Columbia and Cornell are among them.
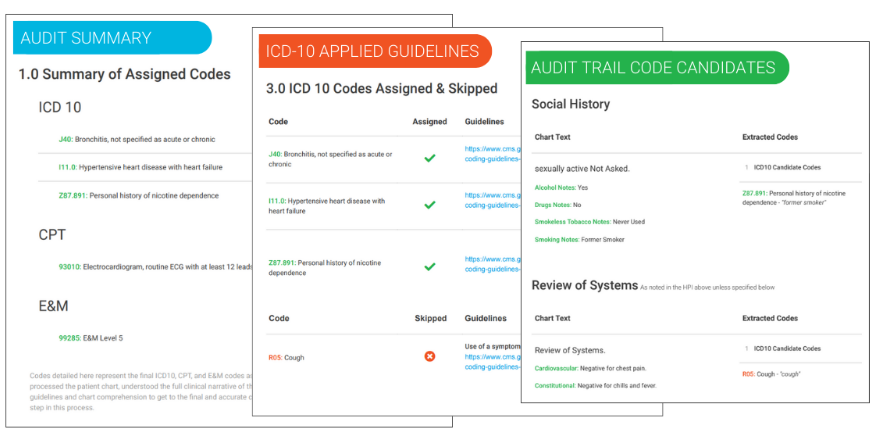 Audit trails make the coding process transparent
Audit trails make the coding process transparent#5 Milagro
- Funding: $9M
- Country: USA
Milagro is an autonomous medical coding solution. It handles multiple specialties, including gastroenterology, cardiology, anesthesia, pulmonology, and orthopedics.
The tool integrates into existing systems for coding ambulatory surgeries and procedures. It reads medical notes, H&P, anesthesia, and pathology reports with the help of advanced language comprehension capabilities of AI and automated clinical reasoning engine. After the analysis, the platform chooses relevant CPT/HCPCS codes.
Milagro also detects human errors in coding and potential denials.
Large academic medical centers with hundreds of thousands of annual surgeries report significant increases in billing accuracy and decrease in denial rates while using Milagro.
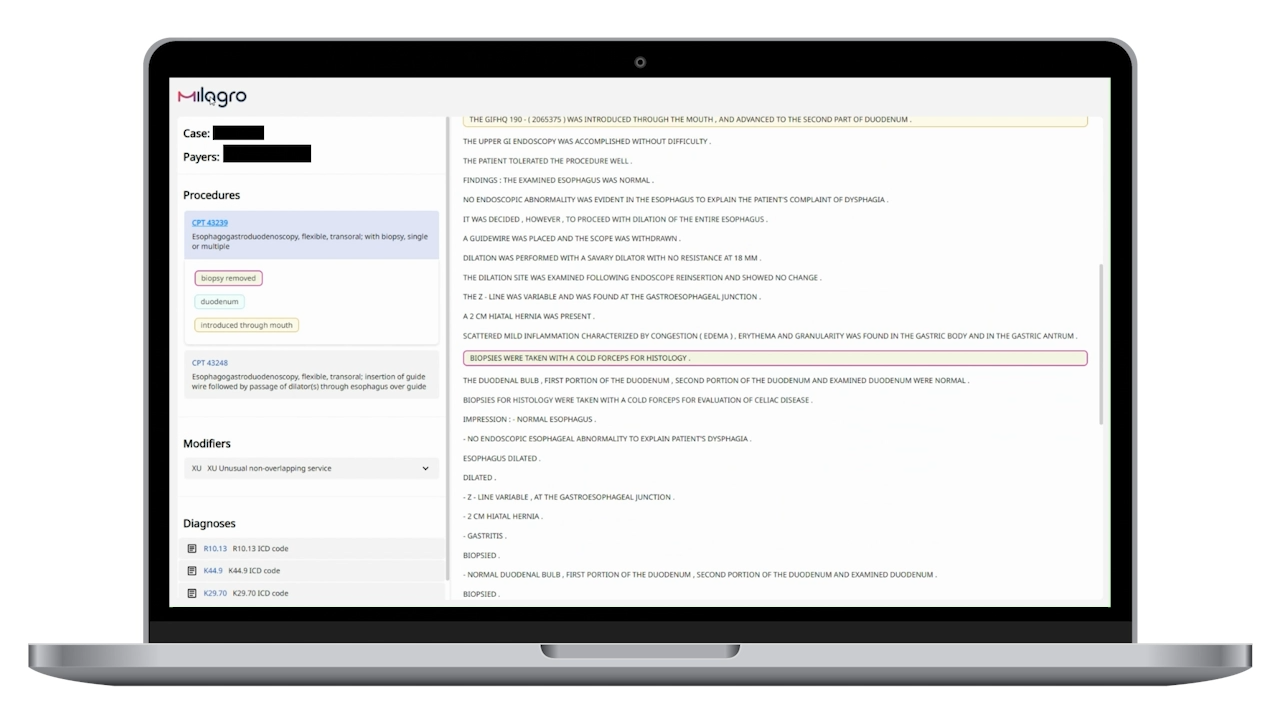 Milagro analyses unstructured medical data and assigns codes
Milagro analyses unstructured medical data and assigns codes#6 Maverick Medical AI
- Funding: $10.2M
- Country: Israel
Maverick’s mCoder platform uses deep learning AI and neural networks to analyze medical documents from EHRs. The platform adapts to different styles of physicians’ notes and understands unstructured medical documentation. After reading the data, the platform performs ICD and CPT coding without the necessity to engage human coders.
Human coders become auditors, which reduces operational costs and speeds up the performance. The process happens automatically and the coding is delivered straight to the billing system.
Maverick is compliant with payor policies.
#7 Synaptec Health
- Funding: $3.3M
- Country: USA
Machine learning algorithms of Synaptec are trained on world’s coding best practices. The platform performs ICD-10, E/M, and CPT coding. It prepares reports about the coded charts.
The tool integrates with healthcare systems using HL7 messaging protocols and supports API integration with formats like JSON. The servers that are compliant with HIPAA read the medical data and generate coded charts ready for billing software in seconds.
The Synaptec team includes physicians, medical coders, engineers, and data scientists.
The solution offers the pay-as-you-go pricing model.
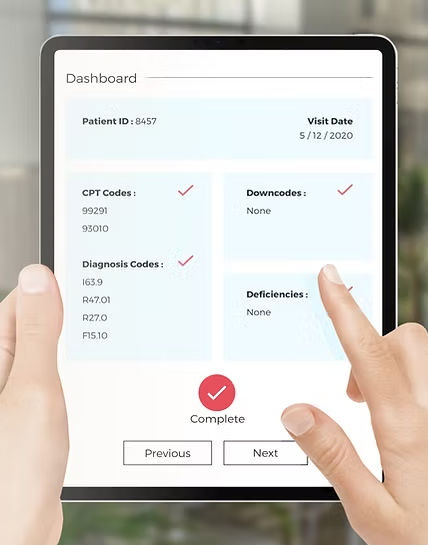 Users verify automatically assigned CPT and diagnosis codes and check the downcodes, and deficiencies
Users verify automatically assigned CPT and diagnosis codes and check the downcodes, and deficiencies#8 RapidClaims
Funding: $3.1M
Country: USA
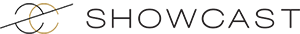
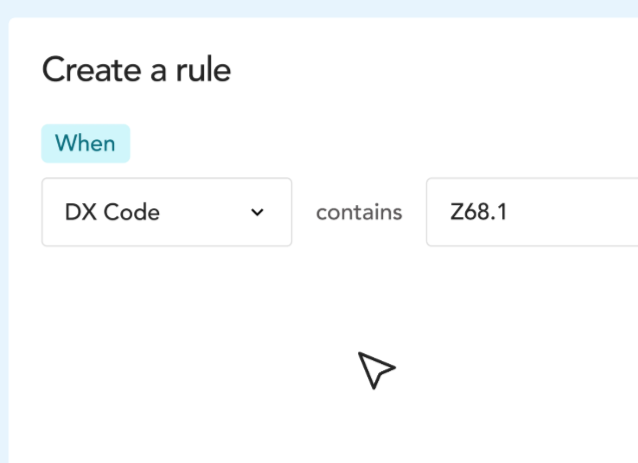
The platform’s AI and LLM read unstructured medical data and convert notes into relevant ICD, CPT, E&M, HCPCS, and HCC codes. It increases the speed of work of in-house or outsourced teams of coders.
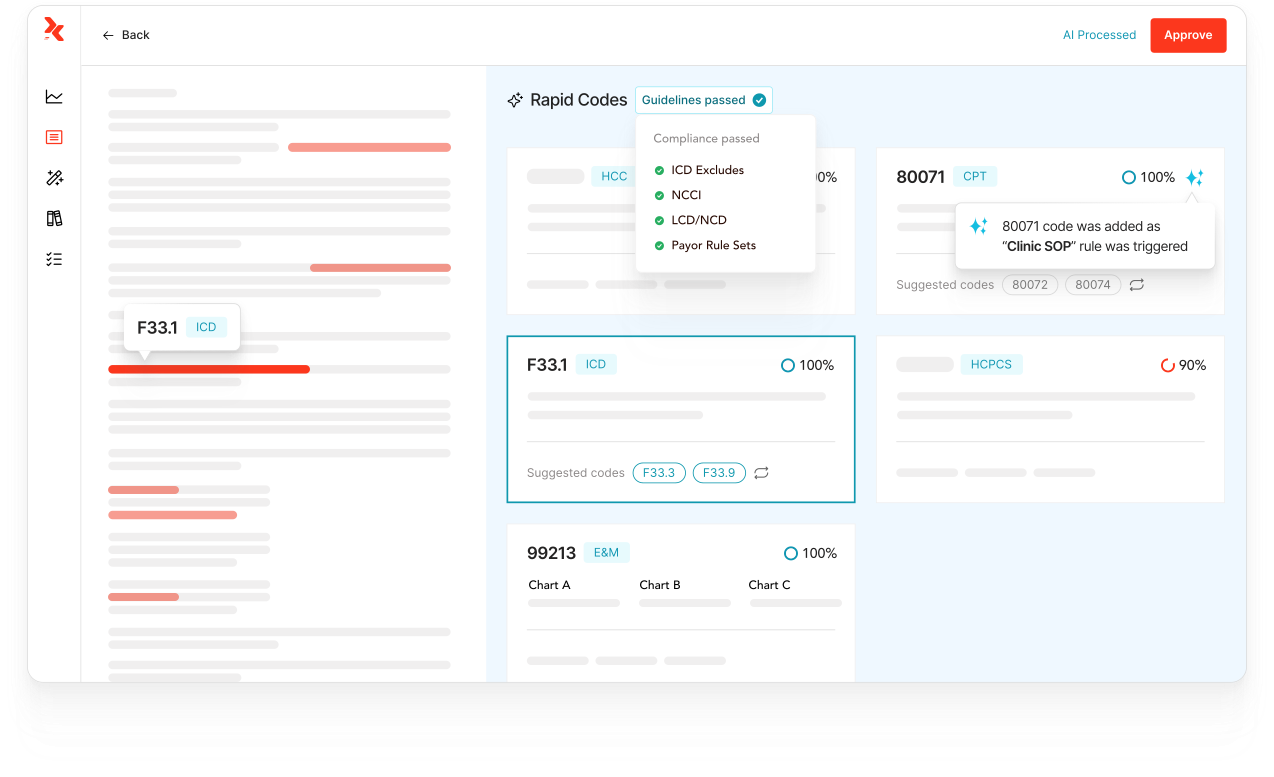
RapidClaims provides audit trails to check the correctness of selected codes. The AI analyzes coding trends and detects claim denial patterns. The solution can also customize coding rules so as not to repeat mistakes.
RapidClaims integrates with Epic, athenahealth, eClinicalWorks, Meditech, and other platforms. It serves nine specialties, including radiology, primary care, labs, nephrology, and ambulatory surgery.
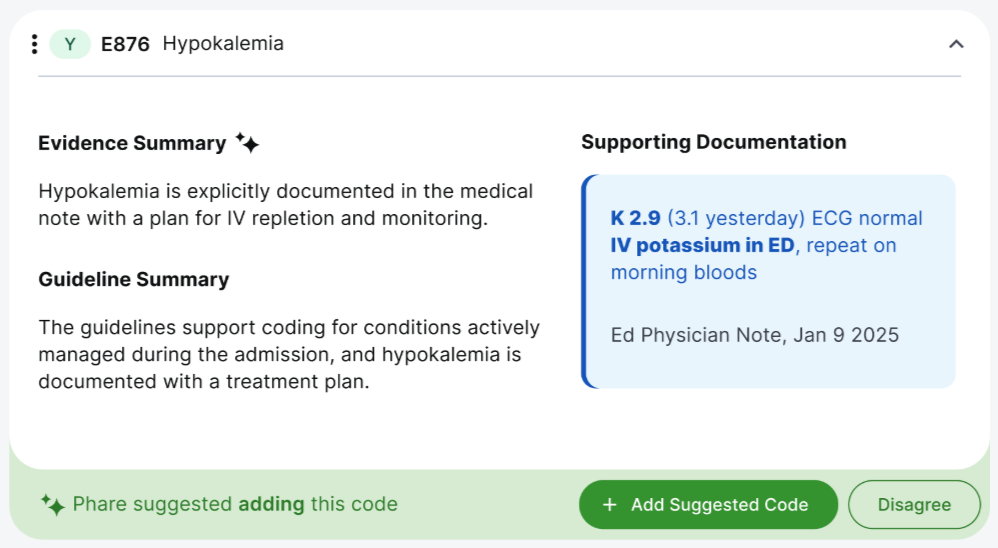
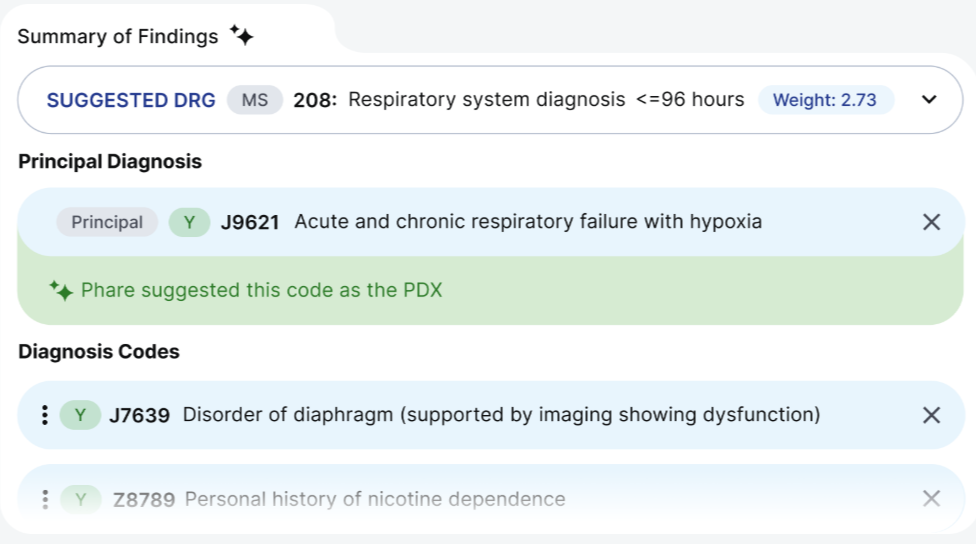
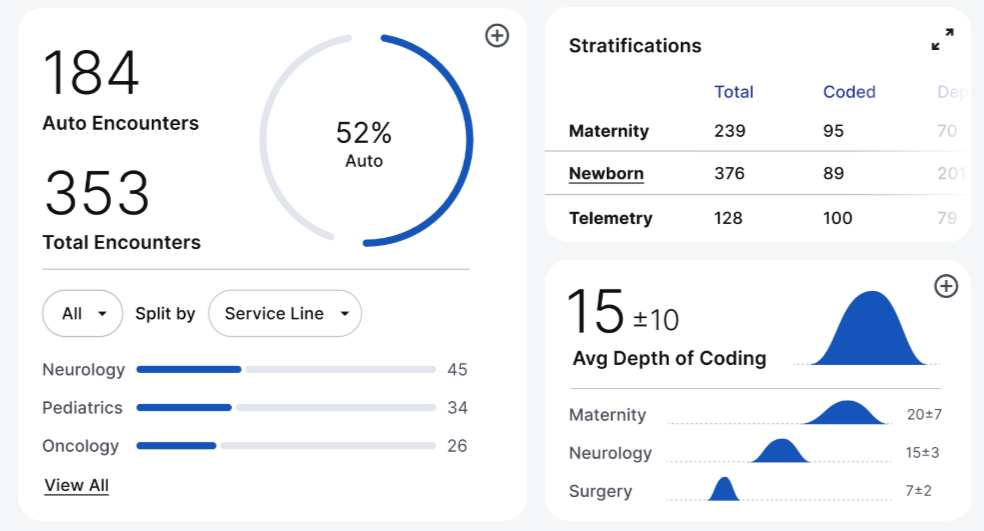
#9 Phare Health
Funding: £2.5M
Country: Great Britain
The company develops AI tools that automate administrative tasks and perform medical coding. Their solutions scan all the clinical data regarding each patient.
The choice of each code is verified with guidelines, best practices, and relevant policies.
The final code list contains audit trails.
#10 Semantic Health
Funding: $2.7M
Country: Canada
Semantic Health uses custom clinical AI and NLP for medical coding and auditing. The algorithms suggest codes and support it with relevant documentation. It results in 100% pre-billing audit coverage. The process applies for all types of insurance payers, specific Diagnosis Related Groups (DRGs), procedures, and diagnoses.
The platform is used in Canadian and American hospitals. It integrates with popular EHRs like Cerner, Meditech, Epic, and others. The platform helps auditors focus on CDI opportunities while the coding is done automatically.
The solution is deployed into the SOC2-compliant cloud environment provided by Microsoft Azure.
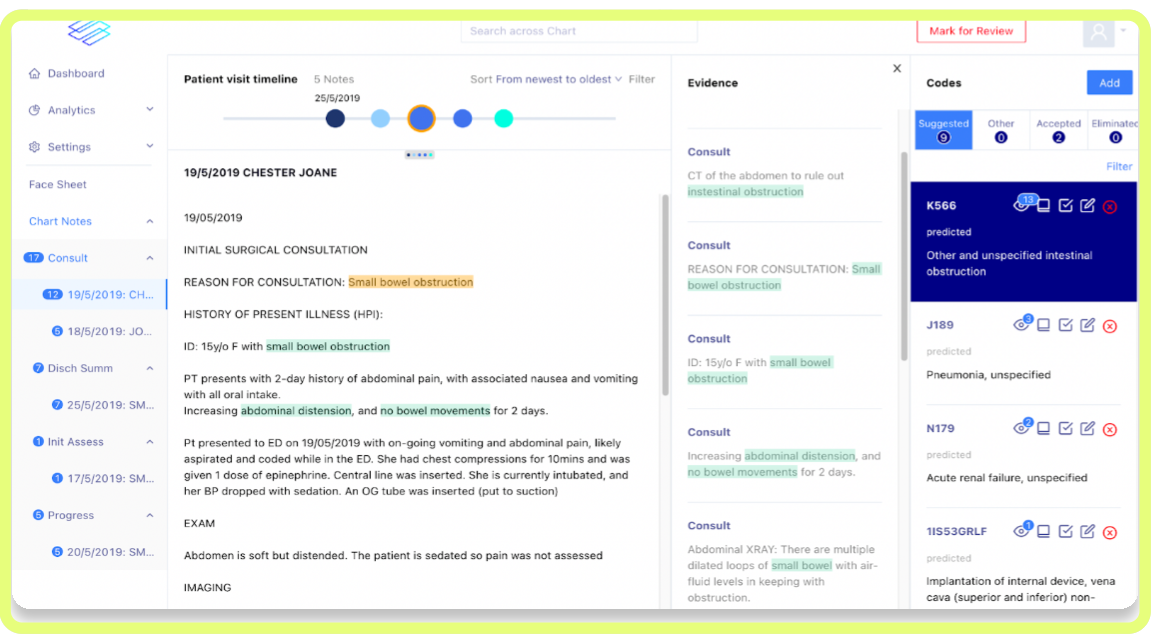 Semantic Health user interface shows patient visit timelines, doctor notes, and suggested medical codes
Semantic Health user interface shows patient visit timelines, doctor notes, and suggested medical codes#11 XpertCoding
Funding: $1.1M
Country: USA
It is a product of XpertDox. XpertCoding is a medical coding engine that uses AI, NLP, and big data analytics. The solution combines medical coding with the BI platform. It monitors coding accuracy and revenue metrics. The system also provides CDI feedback and alerts about issues and discrepancies in the CPT codes.
XpertCoding features payor-specific coding, i.e., aligning billing processes with certain rules and contracts of different payors.
The platform integrates with eClinicalWorks, athenahealth, Epic, and Experity. The Robotic Process Automation allows for two-weeks implementation into the existing EHR.
Leading healthcare companies, such as Stanford Medicine, Northside Medical Professionals, Pediatric Care, Lifespan, and others trust XpertDox and its solutions.
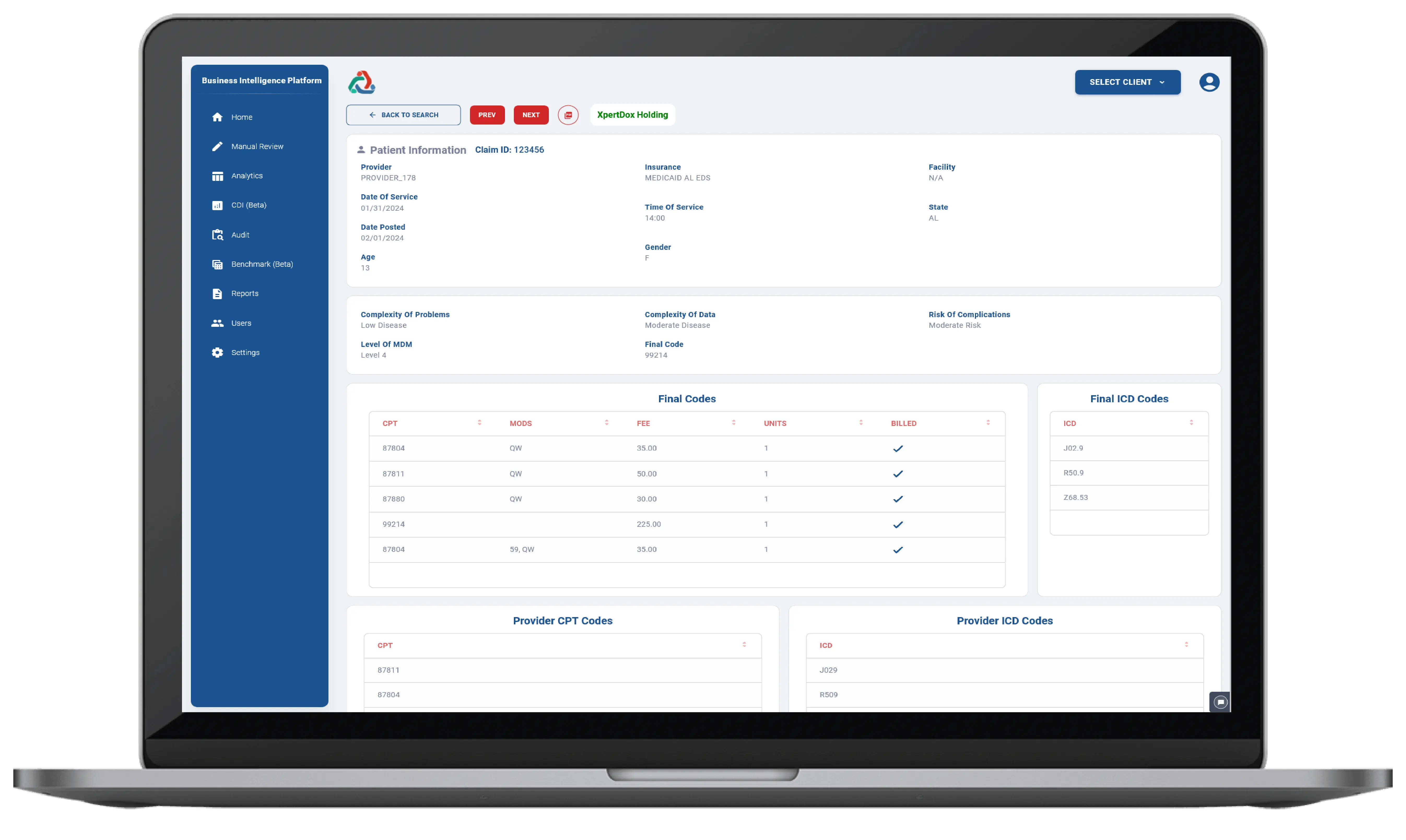 The screenshot of the XpertCoding Audit Trail showing patient information, assigned medical codes (CPT and ICD), and billing details
The screenshot of the XpertCoding Audit Trail showing patient information, assigned medical codes (CPT and ICD), and billing detailsThe Challenges of Medical Coding
Up to 30% of manually coded claims are denied, and up to 65% are never reworked, negatively affecting revenue cycles.
Staffing shortages and high turnover increase Discharged Not Final Billed rates. 55% of healthcare finance leaders report shortages in billing roles. 96% of revenue cycle leaders attribute claim denials (a DNFB driver) to staffing shortfalls.
Delays
Healthcare networks may handle a few million patient visits each year, including hundreds of thousands of emergency department visits. Manual end-to-end workflows (chart reviews, claim submissions, denials management) create systemic delays. It typically takes 5–7 days due to human review, code assignment, and system entry.
Patient volumes double during the winter flu season or holiday staffing shortages, cause the medical coding backlog to grow, leading to delays of weeks.
High costs
Some organizations attract outsourced medical coders. However, the contracts might appear costly. Other coding costs include overtime requirements for in-house medical coders. Besides, they often face limited paid time off (PTO) due to large workloads, which results in work-life imbalance and burnout.
Complex Medical Coding Workflow
Traditionally, medical coding involves certified coders who manually review patient records and relate those records with the most relevant ICD-10 and CPT codes for billing. The US system of codes for medical diagnosis includes more than 70,000 unique codes, and that number is growing by hundreds of new codes annually. Consequently, manual medical coding is time-consuming, error-prone, and costly, especially for high-complexity procedures, such as surgeries or inpatient visits.
Inefficiency of traditional AI tools
Medical coding requires a high accuracy of 95% or higher to avoid claim denials or delays. However, existing large language models (LLM), such as GPT-3.5, GPT-4, Gemini Pro, and Llama2-70b Chat fail to generate ICD-9-CM, ICD-10-CM, and CPT codes with accuracy of above 50%.
Difficult medical terminology
Physicians use specific medical terms, abbreviations, and may describe context-dependent details. Their language may include negation, subjective tones, and other linguistic peculiarities. Therefore, it becomes challenging for traditional natural language processing algorithms to understand the context and accurately select medical codes. While the process of searching the codes becomes automated, the need to validate the data before sending it to billing remains.
Necessity to review and edit coding
With a traditional NLP tool exploited, healthcare organizations have to allocate reviewers who check the coding and validate it. Studies report a drop in productivity when medical coders have to validate and correct suggested codes.
Addressing the Challenges with Custom AI Medical Coding Software Functionality
Automated Medical Coding
AI medical coding software automatically selects the right code for each procedure, and explains why this particular code is assigned. The charts, which are comprehensible to the system, are instantly processed and sent to billing. Unhandled charts are labeled and transferred to human coders for processing.
FHIR integration
Powerful coding software relies on Fast Healthcare Interoperability Resources (FHIR) to receive patient information from EHRs in a quick and secure manner and in various formats. Patient charts are sent in FHIR files across any health system without the necessity for setting additional engine configurations.
Clinical language analysis
AI software examines patient data and determines various sections of patient charts, such as clinical notes and structured data, e.g., medicines, laboratory results, screenings, etc. This is done with the help of content-aware machine learning models with linguistic understanding capabilities that are developed specifically for major EHRs (Epic, Oracle Cerner, etc.).
After identifying patient chart sections, the software “reads” and understands syntactic elements of the records, medical concepts, temporality of the concepts, their subjectivity or objectivity, negation, and other linguistic peculiarities. The LLM leverages linguistic rules that result in accurate coding.
Specific language models
Customized AI-based medical coding systems learn from patterns in the data and users’ practices. The algorithm examines the information in the integrated EHR. It studies diagnoses, procedures, and treatments, as well as historical coding data, coding regulations, and guidelines. Based on the input, ML tools can recognize patterns, make predictions, and generate codes.
Benefits of AI Medical Coding Software for Health Systems
- Hundreds of thousands dollars are saved by reducing annual medical coding costs due to removed overtime requirements for in-house coders and eliminated contracts with outsourced coders.
- Hundreds of thousands saved thanks to reduced full-time employee hours.
- Decreased coding backlog and decreased DNFB rates leading to accelerated payment cycles.
- Increased average charges per patient due to more careful procedures recording, capturing complex cases, and consistent charge documentation.
- Improved work-life balance of in-house coders due to relieved workloads.
How Belitsoft Can Help
Get tailored and highly scalable AI medical coding software developed with unique functionality by partnering with Belitsoft developers.
We train and fine-tune AI coding systems to make sure the solution meets your organization’s specialty-specific needs, can quickly code encounters without human intervention, can handle peak volumes, and provides tools to monitor and audit coding outputs.
If your autonomous medical coding company automatically translates clinician notes into billing codes, you need to work with EHRs using deep learning engines and handle terabytes of unstructured, and privacy-sensitive data, which is a significant infrastructure challenge.
- Our senior infrastructure engineers build and maintain scalable systems using Google Cloud, AWS or Azure, Docker, Kubernetes (to orchestrate containers), Spark (to process large datasets in parallel), CI/CD, and MLOps tools (to deploy and manage large-scale applications and integrate ML models into production). They design systems that are secure (HIPAA-compliant), reliable, and capable of handling high loads.
- Our backend/data engineers design data pipelines (ingesting, sanitizing, normalizing, and transforming medical data from various sources like EHRs, journals, etc. into a unified format) with encryption, access controls, audit trails, etc., and build interfaces for this data while scaling data ingestion alongside machine learning. They rely on their skills in Python, databases, data pipelining, and expertise in healthcare data. They also have experience with large-scale data labeling for training ML models.
If your multi-specialty AI medical coding engine company processes millions of medical charts across healthcare facilities to understand clinical language and automate medical coding, you may need a scalable infrastructure and someone who can handle reliability issues.
- Our backend & DevOps engineers use Python for data processing and integrating ML models, maintain CI/CD pipelines (Jenkins or GitHub Actions) for continuous deployment and integration—which is important for frequent updates without downtime—and configure Infrastructure-as-Code (IaC) to make your cloud environments reproducible and scalable.
- Our database software engineers develop features from design to implementation, relying on their RDBMS experience (Postgres, MySQL) to handle structured data from EHRs. They design database schemas, optimize queries, and do integration work with the autonomous engine, so it can access and store data. They also integrate backend services with the database, enabling the system to handle high transaction volumes.
- To customize your coding engine according to your client's needs, our medical data analysts—skilled in SQL and Pandas (Python), with expertise in medical terminology, U.S. EHRs, and revenue cycle management—are at your service.
If your pioneering team is revolutionizing healthcare with AI-driven medical coding using NLP and machine learning, you may have a web application with a user interface where healthcare providers interact with the system and understand the importance of the web app's usability.
- Our senior full-stack engineers work with the latest versions of modern frontend frameworks (Angular, TypeScript, etc.) and backend technologies (Golang, Node.js, Express.js, etc.) to build scalable SaaS apps in a cloud-native environment (AWS with services like DocumentDB, DynamoDB, Cognito, SQS, etc.), using the Vibe Coding method for faster, more automated development. They perform automated pre- and post-deployment tests, integrate REST APIs and third-party services with interoperability in mind, and are comfortable with high-performance architectures, distributed computing, and parallel processing.
Rate this article
Recommended posts
Our Clients' Feedback
















.jpg)
.jpg)
.jpg)
.jpg)
.jpg)
.jpg)
.jpg)
.jpg)
.jpg)
.jpg)
.jpg)
.jpg)
.jpg)
.jpg)
.jpg)
.jpg)
.jpg)
.jpg)
.jpg)
.jpg)
.jpg)
.jpg)
.jpg)
.jpg)
.jpg)
.jpg)
.jpg)
.jpg)
.jpg)
.jpg)
.jpg)
.jpg)
.jpg)
.jpg)
.png)
.jpg)
.jpg)
.jpg)
.jpg)
.jpg)
.jpg)
.jpg)
.jpg)
.jpg)
.jpg)
.jpg)
.jpg)
.jpg)
.jpg)
.png)
.jpg)
















We have been working for over 10 years and they have become our long-term technology partner. Any software development, programming, or design needs we have had, Belitsoft company has always been able to handle this for us.
Founder from ZensAI (Microsoft)/ formerly Elearningforce