The growth rate of payment integrity software will decrease from 28% to 13% GAGR in the coming years but will still remain significant. It's used to ensure accurate claims processing, detect fraud, and prevent improper payments by healthcare payers (insurance companies, government programs like Medicare/Medicaid, and managed care organizations).
What Is Payment Integrity?
Payment integrity is the process of ensuring that a payment is proper. It requires strong documentation and coding processes.
Payment integrity includes prepayment and post-payment approaches.
Prepayment capabilities proactively identify and correct billing errors before the payment is processed. Post-payment capabilities find and resolve past payment errors.
The traditional approach implies that payment integrity audits are completed after the care has been provided and the claim has already been paid. Such a post-payment approach results in administrative costs and troubles for providers and payers.
A proactive process eliminates improperly documented claims before they are paid. Such solutions also check that claims are paid according to the contractually agreed price between the health plan and the care delivery organization.
Challenges of Healthcare Payments
Payment and financial challenges
Coding and clinical documentation mistakes lead to recouped payments, denials, and legal issues.
Healthcare systems fail to visualize possible reliances between payment term changes and reimbursements or savings. Lack of timely and accurate details negatively impacts the understanding of financial implications and particular contract terms.
Recurring payment errors appear due to the absence of a relevant tool to address root causes.
Technology and software limitations
The available software does not always mean that it can scale with the organization's needs.
Many health plans still use legacy tools, e.g., pivot tables and spreadsheets to review contract scenarios. Manual solutions cause errors, demand much time, and lack flexibility.
Workflow integration issues
Hampered data flow between platforms disrupts care management teams.
Contract negotiations require referring to various systems and sources. If those sources are disjointed, it hampers the analysis process and complicates workflows.
Agreements between payers and providers may fail to fit existing claims processing systems. Such problems lead to operational bottlenecks and implementation delays.
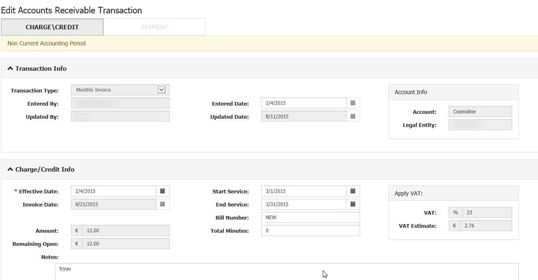
Payment Integrity Software Functionality
Customized payment integrity software solutions might offer the following capabilities:
Financial analytics and transparency
The software predicts reimbursement terms and forecasts the financial impacts of the contracts, improving negotiation transparency.
The software identifies which claims are influenced by provider contract negotiations and implementation, aiding informed decision-making.
Users can set up unlimited payment carveouts, establish payment rules, freeze rates, and handle complex scenarios.
Unified platform functionality
All the processes happen within a single platform, i.e., claims editing, pricing algorithms, and additional analytics solutions function in a cohesive manner, evaluating information and contracts.
Self-service capabilities
Contract negotiation teams can set up, compare, and adjust contract terms independently. The software also allows for building and running “what-if” scenarios and assessing potential consequences without exploiting additional software, such as contract management platforms.
Real-time updates and visibility
The system informs about the claims that are affected by the CMS changes and financial consequences.
Providers see claims edits on the platform. It reduces additional interactions and leads to better visibility.
Documentation and coding support
Doctors use integrated templates to avoid documentation errors and standardize the electronic health record (EHR) data.
Integration of computer-assisted coding systems that use artificial intelligence (AI) and natural language processing (NLP) for proper coding. Ambient AI scribes can read clinical notes, suggest appropriate codes, and justify those suggestions.
Performance measurement
Setting the KPIs, such as discharged not final billed (DNFB) rates, denial rates, underpayment recoveries, and avoidable write-offs as a percentage of revenue, etc. enable providers to track the measures and analyze claims data correctly.
Users analyze every processed claim and generate benchmarks that can be categorized by various measures in holistic reports.
How Belitsoft Can Help
Healthcare software development companies like Belitsoft provide healthtech startups with expert assistance in creating, customizing, and supporting payment integrity software with capabilities that include, but are not limited to, the following:
- Data consolidation and integration from various sources.
- Built-in data quality tools.
- Reliable API integration.
- User-friendly interface.
- Predictive analytics to assess the risks of suspicious activities.
- Embedded personalized templates for doctors to compile error-free clinical notes.
- Integrated AI algorithms and machine learning to enable automatic coding and claims verification.
- Adherence to health systems’ regulations.
If you're looking for expert assistance in data infrastructure, data platforms, workflow engineering, and cloud development (including AWS, Azure, and Google Cloud), as well as hybrid or on-premises environments, the Belitsoft healthcare software development company offers outsourced expertise to meet your needs.
Rate this article
Recommended posts
Portfolio
Our Clients' Feedback
















.jpg)
.jpg)
.jpg)
.jpg)
.jpg)
.jpg)
.jpg)
.jpg)
.jpg)
.jpg)
.jpg)
.jpg)
.jpg)
.jpg)
.jpg)
.jpg)
.jpg)
.jpg)
.jpg)
.jpg)
.jpg)
.jpg)
.jpg)
.jpg)
.jpg)
.jpg)
.jpg)
.jpg)
.jpg)
.jpg)
.jpg)
.jpg)
.jpg)
.jpg)
.png)
.jpg)
.jpg)
.jpg)
.jpg)
.jpg)
.jpg)
.jpg)
.jpg)
.jpg)
.jpg)
.jpg)
.jpg)
.jpg)
.jpg)
.png)
.jpg)


















We have been working for over 10 years and they have become our long-term technology partner. Any software development, programming, or design needs we have had, Belitsoft company has always been able to handle this for us.
Founder from ZensAI (Microsoft)/ formerly Elearningforce