Let’s take a look at how FHIR’s transformative technology inspires many applications to emerge on a global scale.
FHIR introduces a standard whose elements (resources) are represented in JSON format and accessed using RESTful API. It is a global health interoperability standard that promotes scalable sharing of individual patient records across the entire healthcare system, moving away from proprietary data models towards common data models. FHIR provides a framework for data exchange through open APIs. It encompasses patient care, administration, payment, and the representation of medical research. In the USA, the federal government has driven the adoption of FHIR, beginning with the 21st Century Cures Act, which mandates API access for patients to their medical records. FHIR-based projects have also been implemented in Eropean countries (e.g., Denmark and Switzerland), Australia, and New Zealand. It is also supported by the World Health Organization.
DICOM on FHIR
DICOM is the international standard for medical images, ensuring interoperability across devices and systems. It is widely implemented in radiology, cardiology, and other medical domains. Hospitals worldwide use DICOM for producing, storing, displaying, sending, querying, processing, retrieving, and printing medical images. By grouping information into data sets—including patient ID, image pixel data, and metadata—DICOM ensures that medical images are always linked to the correct patient and context.
To integrate medical imaging with broader clinical workflows, FHIR provides the ImagingStudy resource. This resource acts as a bridge between DICOM imaging data and FHIR’s clinical data model. It includes metadata about DICOM imaging studies, such as DICOM Unique Identifiers (UIDs), device type codes, and references to patient data.
It also provides an URL for retrieving images via DICOMweb, enabling access to medical images within FHIR-based systems.
DICOMweb provides a family of RESTful services for sending, retrieving, and querying medical images and related information. The principal services include WADO-RS for retrieval, STOW-RS for storage, and QIDO-RS for querying. These services make DICOM data accessible via web-based APIs, aligning with modern interoperability standards.
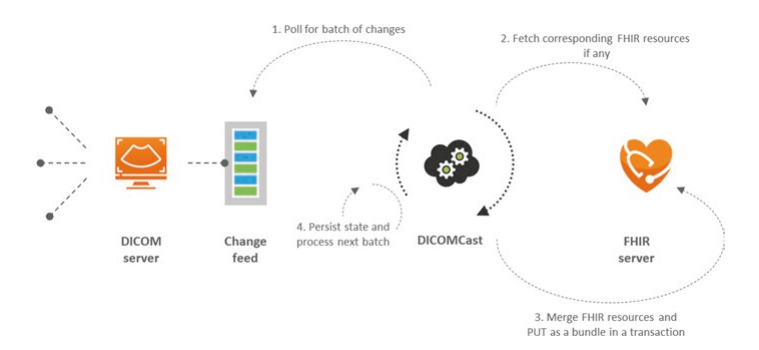
To further integrate DICOM and FHIR, Microsoft has developed the Medical Imaging Server for DICOM, an open-source DICOM server that supports standards-based communication with DICOMweb-enabled systems. Alongside this, Microsoft’s DICOM Cast tool polls changes in a DICOM server and transforms them into FHIR resources (e.g., Patient and ImagingStudy). This integration enables a holistic view of patient data by combining imaging and clinical information within FHIR-based systems like Azure API for FHIR.

InteropEHRate Patient App
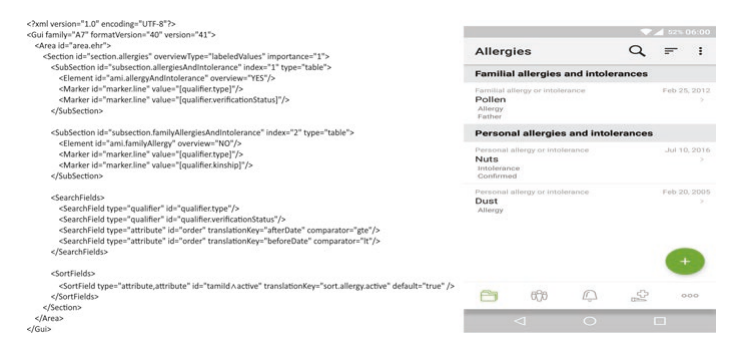
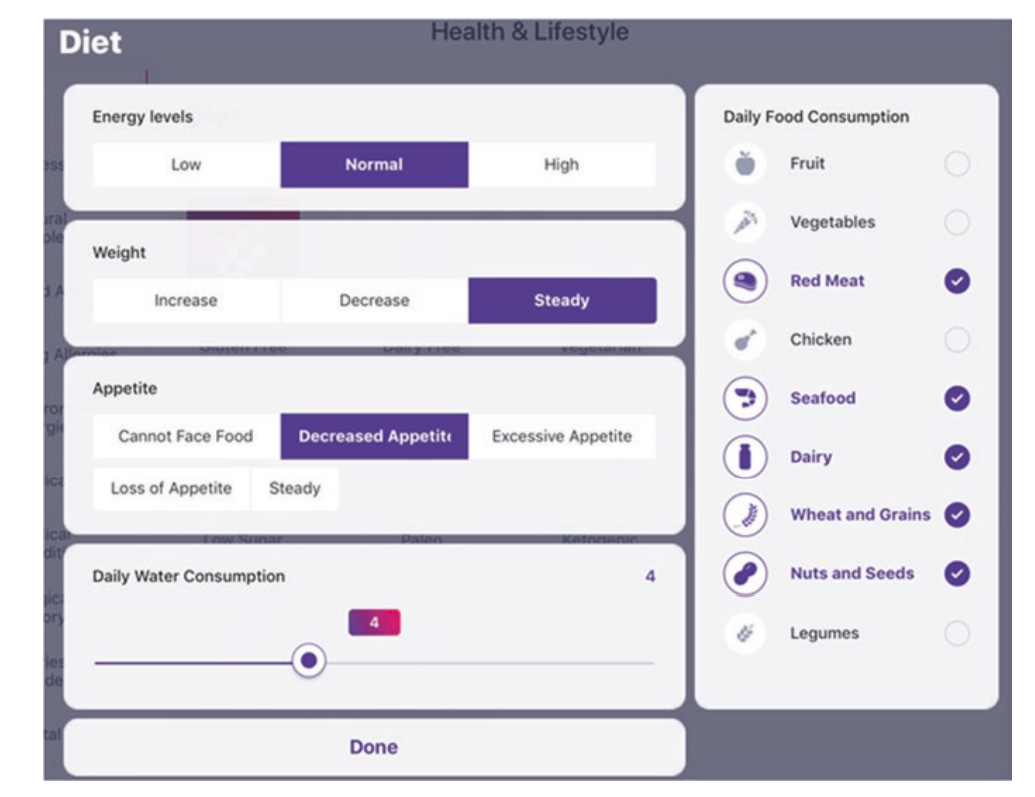
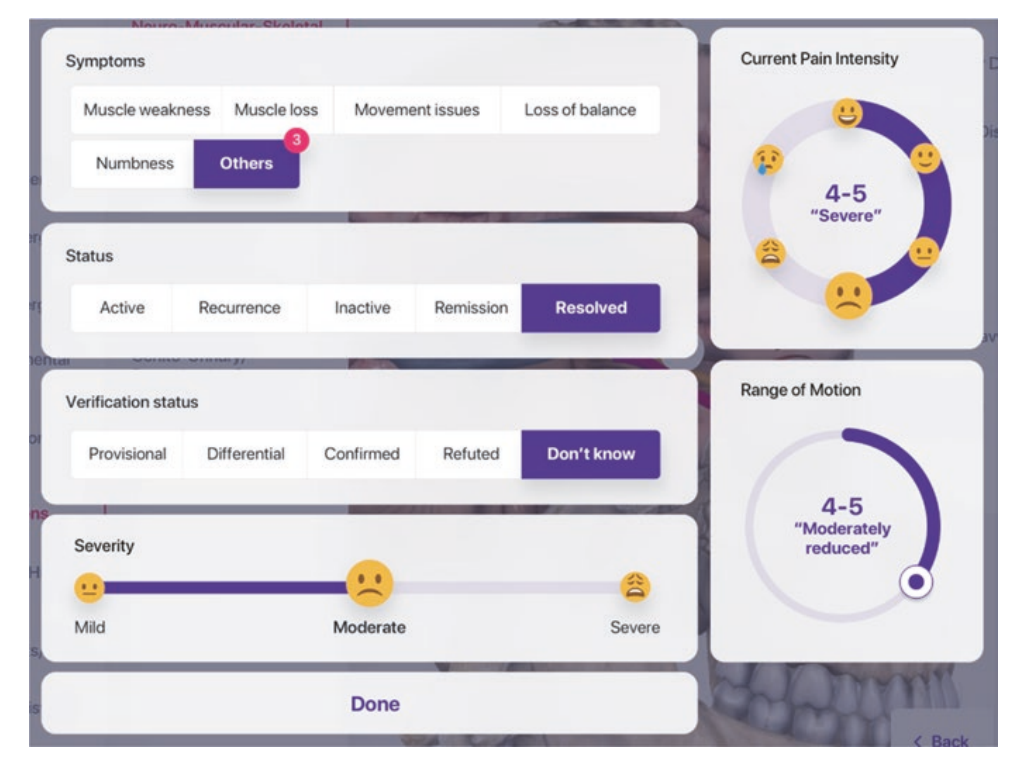
Andaman7 is an example of implementing FHIR to build a patient-driven mobile Personal Health Record (PHR) and an intermediation platform for secure health information exchange. The goal is to allow everyone to manage their health information on their mobile devices and to share it freely, particularly for research. Andaman7’s revenue is derived from providing electronic questionnaires for data collection for decentralized clinical trials.

In the US, users of the app can download their EHR records from various intermediaries, like Apple using the mapping to HealthKit. Apple has connected to thousands of hospitals and health care providers using FHIR, so the data is available to iPhone users via the company’s HealthKit. Andaman7 also offers all its users, independent of their phone type, EHR access via other intermediaries’ (such as 1upHealth) connections to the FHIR gateways of many US healthcare facilities. These connections currently exist only in the US.
The InteropEHRate effort is designed to provide patients with a personal health record across all the European Union countries. Here, Andaman7’s app uses InteropEHRate protocols, which are based on FHIR, to connect to healthcare professionals or organizations via classic internet connections or via a local Bluetooth connection (e.g., in the physician’s office before or after a visit).
Platforms
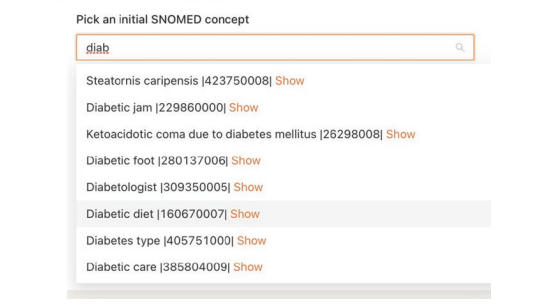
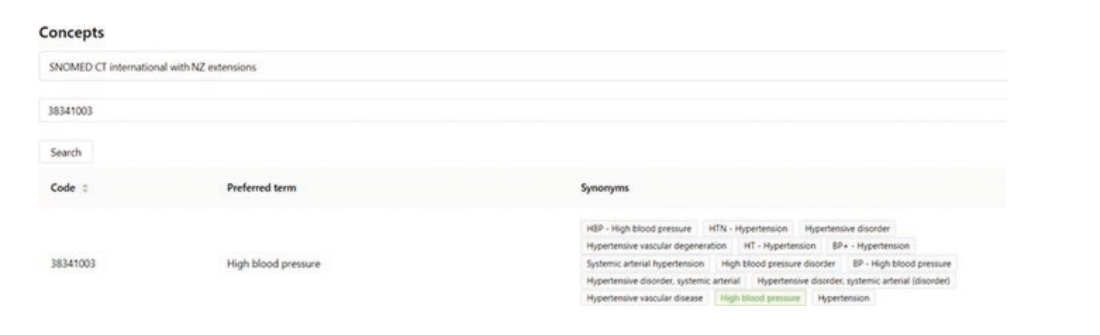
New Zealand is building an API infrastructure as part of its digital health ecosystem, primarily using the FHIR standard and SNOMED CT for terminology.
This initiative requires APIs for all new systems and retrofitting APIs to update existing systems. It also establishes a record locator service to securely index health information from trusted sources, making it accessible in a controlled manner. Additionally, it creates a pool of reusable integration components, algorithms, and program code around keyservices and the national health information platform.
Local companies develop applications that comply with the government’s requirements for using FHIR and SNOMED CT and participate in projects like ACC-45 Injury Claims, which integrate into New Zealand’s national healthcare system.
One of the applications is a FHIR platform.
FHIR Questionnaire and QuestionnaireResponse Resources
This application uses FHIR standards for efficient data collection during patient check-in. Patient medical history from the electronic medical record is converted into a QuestionnaireResponse format to pre-fill check-in forms, reducing manual data entry. Patients provide updated information during check-in, which is stored using the FHIR QuestionnaireResponse resource.


Since QuestionnaireResponse stores unstructured data, then it is processed and transformed into structured FHIR resources (e.g., Patient, Observation) for compatibility with the EMR. The structured data from the check-in process is integrated back into the patient’s EMR, ensuring their medical history stays up to date and accurate.
Clinical Notes Consultation
A clinical notes consultation module allows a clinician to document care by annotating a photo of the patient’s face. AI and ML are used to automatically detect the anatomical structures of the facial anatomy in the photo of a patient.
The clinician uses visual tools to capture the entire treatment encounter by annotating the photo to document procedures carried out as well as devices and medications used, with no need to type or write clinical data.
This information is converted to SNOMED codes, structured into various FHIR Procedure resources that are linked to a FHIR Encounter resource that becomes part of the record. By capturing clinical data in such a highly structured form, the app may eventually predict the best treatment plan for a patient based on numerous factors such as age, race, facial shape, skin type, and more. This technique might also be used to monitor wounds on various body structures postsurgical patients in the future.

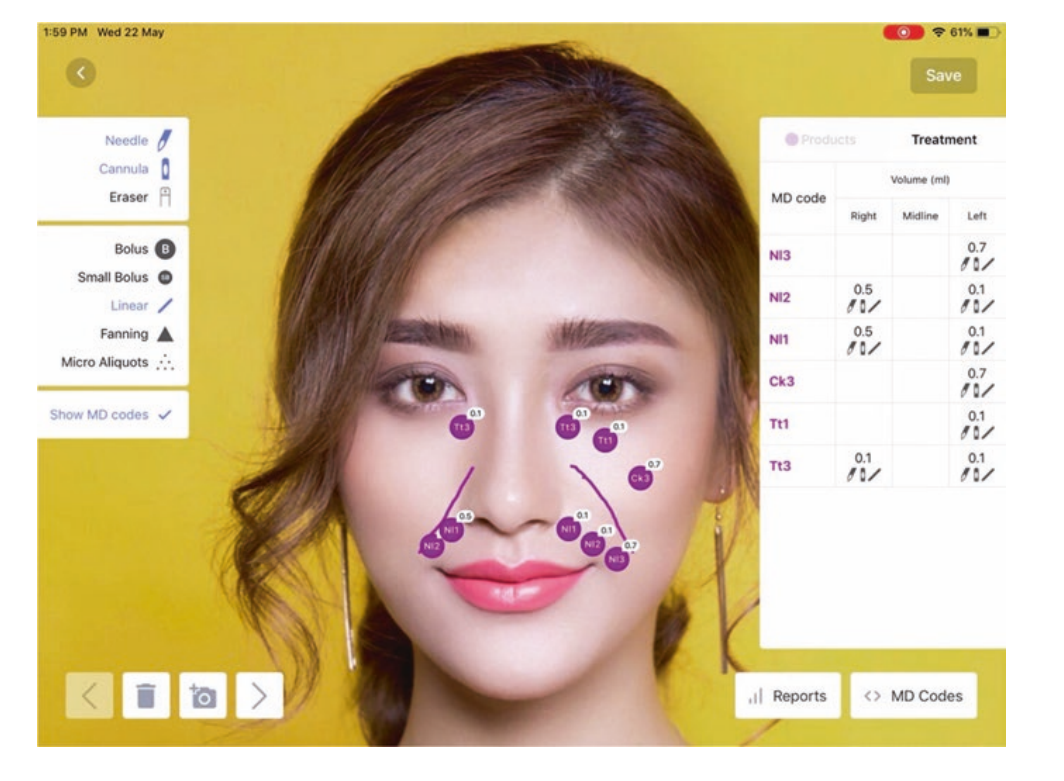

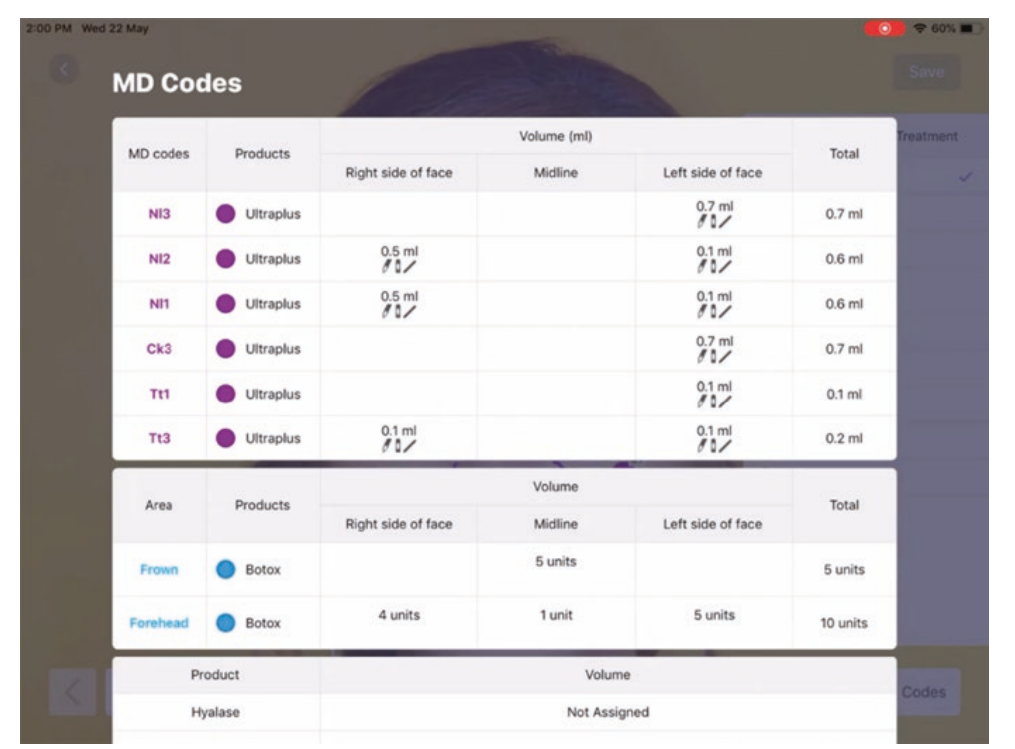
The visual annotations are converted to SNOMED codes, structured into various FHIR Procedure resources that are linked to a FHIR Encounter resource that becomes part of the record.


mCODE and CodeX: A FHIR Standard for Cancer Care
The data for the majority of cancer patients is stored in electronic health records (EHRs), often in unstructured formats like free text. Making EHR-based patient data useful for cancer research requires a common standard and language for oncology.
The Minimal Common Oncology Data Elements (mCODE) is an HL7 FHIR Implementation Guide representing a core set of structured data elements for digital clinical oncology data.
CodeX (Common Oncology Data Elements eXtensions), an HL7 FHIR Accelerator project, was formed to build a community to facilitate interoperable data modeling and applications based on mCODE.
It is developing supplemental Implementation Guides for use cases, such as:
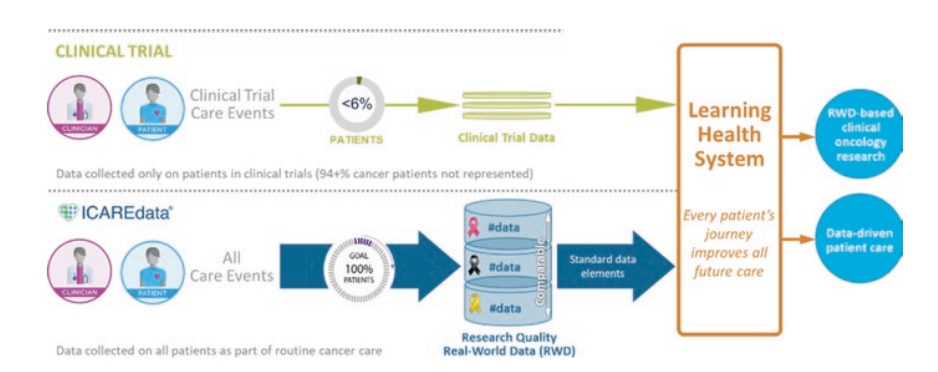
- ICAREdata Project. Integrating clinical trials and real-world endpoints to demonstrate that EHR data can be structured and contribute to efficient clinical research.
- Trial Matching. Leveraging mCODE open data standards and APIs to enable interoperable, scalable, and accessible clinical trial matching services.
- Registry Reporting. Enabling low-burden, mCODE-based reporting of cancer data from cancer centers to registries.
- Radiation Therapy Treatment Data. Developing open data standards based on mCODE for interoperable exchange of radiation therapy treatment summary data.
- Prior Authorization in Oncology. Using mCODE-based health data to enable prior authorization auto-approvals.

SMART on FHIR App for Medication Management
MedWise clinical decision support tools demonstrate how FHIR technology can enhance electronic health record (EHR) connectivity. Pharmacists and clinicians nationwide access MedWise via the company’s SMART FHIR app to promote safer medication use and improve prescribing practices.
The MedWise medication management solution enables healthcare providers to comprehensively analyze complex drug regimens and optimize patient medication regimens. It helps pharmacists identify and address medication-related risks across a variety of safety factors, making it a potentially lifesaving tool.
MedWise provides a holistic view of a patient’s entire medication list. It performs concurrent analyses that consider pharmacokinetics (what the body does to the drug), pharmacodynamics (what the drug does to the body), pharmacogenomics (the impact of an individual’s genomic makeup), and Chronopharmacology (how drug administration timing impacts metabolization and effects). This comprehensive screening helps identify accumulative multi-drug interactions, enabling clinicians to assess simultaneous interactions in a single view. The goal is to mitigate risks, simplify complex medication science, and support safer prescribing while minimizing alert fatigue.
The platform includes powerful decision support tools, such as:
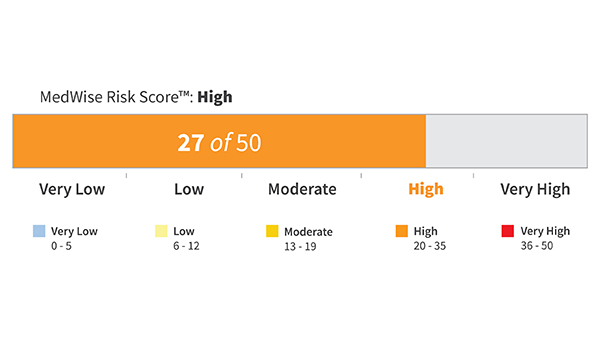
- MedWise Risk Score (MRS): A numerical indicator of a patient’s risk, calculated using the active ingredients in their entire medication profile. The MRS guides recommendations and benchmarks intervention impact.
- Adverse Drug Event (ADE) Bullseye and Side-Effect Wind Rose Diagrams: Visual tools providing at-a-glance, actionable insights into patient risks.
- Medication Risk Mitigation (MRM) Matrix: A schematic representation of a patient’s medication list for deriving personalized safety guidance, including drug-gene and multi-drug interactions.
When patient genomic information is included, MedWise delivers even more precise and personalized care, incorporating drug-gene interactions and phenotype conversions into the analysis.
MedWise is a cloud-based platform that leverages FHIR for integration and bidirectional communication with clinical call centers, pharmacies, health plans, and insurance providers. It supports connectivity with robotic dispensaries and facilitates real-time data sharing between platforms.
FHIR is central to MedWise's integration with electronic medical record (EMR) systems and health service applications. It enables real-time access to clinical, pharmacological, and pharmacogenomic data. FHIR is used to obtain medication lists, demographics, eligibility information, and patient-specific data when launching MedWise tools within host applications or synchronizing data between systems.



Evidence-Based Medicine on FHIR
Clinical decisions should be supported by accurate, timely, and up-to-date information and should reflect the best available evidence. This means integrating individual clinical expertise with external clinical evidence derived from systematic, clinically relevant research, particularly patient-centered clinical research. It requires skills such as efficient literature searching and basic abilities in interpreting epidemiological and statistical results. However, even a skilled searcher can face an overwhelming set of results. Furthermore, reviewing the evidence, even when links are provided, can be a time-consuming process, which is problematic for busy clinicians. A FHIR-based schema could facilitate this process.
EBMonFHIR is a project that uses FHIR to create a system linking medical research with patient data. The goal is to provide clinicians with up-to-date scientific evidence for real-time decision-making. This solves the problem of inefficient search and processing of medical literature, which is often not available in a machine-readable format. The project uses FHIR Resources (e.g., EvidenceReport, Evidence, Citation) to structure research data. EBMonFHIR integrates research data with EHR via FHIR. The project demonstrates how FHIR can be used to create clinical decision support (CDS) systems.
The project aims to provide interoperability standards for data exchange for those producing, analyzing, synthesizing, disseminating, and implementing clinical research (evidence) and recommendations for clinical care (clinical practice guidelines).
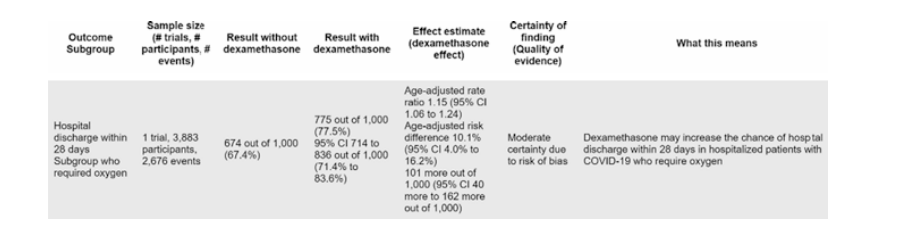
Key tools include the MEDLINE-to-FHIR Converter, which transforms MEDLINE references into FHIR Citation resources, enabling computable access to over 27 million life sciences journal articles, and the ClinicalTrials.gov-to-FHIR Converter, which converts more than 300 data elements from ClinicalTrials.gov trial registers into FHIR resources. The Clinical Trials Results Reporter (CTRR) is a prototype tool for human-friendly data entry and transformation of clinical trial results into computable FHIR resources.

Rate this article
Recommended posts
Portfolio

Our Clients' Feedback
















.jpg)
.jpg)
.jpg)
.jpg)
.jpg)
.jpg)
.jpg)
.jpg)
.jpg)
.jpg)
.jpg)
.jpg)
.jpg)
.jpg)
.jpg)
.jpg)
.jpg)
.jpg)
.jpg)
.jpg)
.jpg)
.jpg)
.jpg)
.jpg)
.jpg)
.jpg)
.jpg)
.jpg)
.jpg)
.jpg)
.jpg)
.jpg)
.jpg)
.jpg)
.jpg)
.jpg)
.jpg)
.jpg)
.jpg)
.jpg)
.jpg)
.png)
.jpg)
.jpg)
.jpg)
.jpg)
.jpg)
.jpg)
.jpg)
.jpg)
.jpg)
.jpg)
.jpg)
.jpg)
.jpg)
.jpg)
.png)
.jpg)
















We have been working for over 10 years and they have become our long-term technology partner. Any software development, programming, or design needs we have had, Belitsoft company has always been able to handle this for us.
Founder from ZensAI (Microsoft)/ formerly Elearningforce