EHRs exist to organize data for legal compliance and facilitate billing processes. Our company customize and upgrade existing EHR systems and create new ones. We have experience developing EHR startups. B2B companies with popular EHR products often come to us. Their users, usually clinic chains, want our clients to improve specific parts for them. Our EHR developers solve all technical tasks, like we did for this EHR client or for this one (a health tech company supported by the U.S. government). Sometimes we even fully update old backends for EHR systems, making our clients' businesses safer and stronger, like we did here.
Belitsoft is a technology partner that has in-depth experience in the healthcare industry and understands the unique challenges of developing EHR systems, a trusted advisor that can help you achieve your strategic goals, and an EHR development company that is able to provide excellent customer support for the long-term.
Hire EHR developers to customize HIPAA-compliant EHR for your healthtech business.
Reasons Behind the Custom EHR Development
The growing demand for security, scaling, and sharing data is causing trouble for those who use legacy EHR Systems. If patient information is spread across incompatible systems, it's difficult to get a complete picture and use real-time updates. Because users have to manually enter data, transferring information between systems leads to errors. Sharing patient data raises concerns about protecting patient privacy and complying with legal requirements. Such EHRs may have weak security, increasing the risk of data breaches or unauthorized access. Many legacy EHR systems have unintuitive interfaces, making them annoying to use.
Organizations that have custom EHR system want modify and expand them on a variety of reasons. They may want get positive net financial return, decrease expenses by participating in state programs (Promoting Interoperability Program, MIPS and the Quality Payment Program) or satisfy the legal requirements ( HIPAA certification, ONC certification) and so on.
“[...] A long-term approach that seeks to achieve small, incremental changes in processes [...] enables organizations to fine-tune their EHRs in response to changing healthcare regulations, new technologies, evolving patient needs and a growing aging population. Without change management, however, the EHR operates in a silo and doesn’t align with the way clinicians practice medicine or with new industry demands, which creates dissatisfaction and underutilized technology.”. KPMG
How we estimate custom EHR development
The cost of EHR development depends on the number of features you need right away - the more of them and the more unique they are (SCOPE), the sooner you need to implement them (TIME) - the more expensive the development is likely to become (COST) (the so-called Quality triangle).
The most expensive part of creating a new EHR is backend and integrations, not user interfaces.
Healthtech companies express interest in our custom EHR development services for the following reasons: proven experience in working with healthcare domain; competitive pricing; good reviews and references available online.
They want to know how much it would cost to customize their EHR systems and see examples of EHR systems we have developed in the past.
In many cases, each customer has their own very specific requirements. We asks our customers to help us clearly identify their needs and requirements to inform our EHR design and development team before the estimation process begins.
After the NDA is submitted, our EHR Business Analyst talks to customers on a video call and asks detailed questions on features of their EHR system to estimate the development costs for each function.
After all the questions have been answered, the information is passed to our Senior EHR Developers. They prepared the “Use-Case Based Requirements Specification” with interactive Figma prototypes.
Based on mentioned documents our proposal includes detailed descriptions of all the features and detailed estimation.
We suggest to split the EHR project development into three main phases in accordance with the hierarchy of goals:
- Proof of Concept (POC). At this stage, we suggest to customize the basic elements of the EHR system. Within this phase, our clients in a cost-effective and timely manner can evaluate our performance and see the first results.
- Minimum Viable Product (MVP). At this stage, we suggest to create the scope of work and prototypes for the things that have not been specified in detail earlier but are required.
- 'Phase 3'. At this stage, we suggest to create other functionality that was not mandatory for the MVP.
The final estimation based on the hierarchy of goals is presented via a video call. Customers invite their own technical specialist to evaluate our EHR team’s skills in the real time.
Often, after that, the budget is approved and the contract is signed.
How we manage custom EHR development
The Agile software development process is often chosen because our clients want to build a large and complex software product while being highly involved in the project development and customization. At its core, Agile is a software development methodology that make it possible to quickly change the EHR software in accordance with business changes.
Effective communication is always 50-60% of a successful custom application development, that is why we establish a proper communication plan.
- The communication is mostly remote. The client can visit the Belitsoft office before the development process begin, if necessary.
- The EHR software development process is often divided into sprints - periods of time during which a portion of programming work has to be completed and be ready for the client’s review. We prepare e-mail reports for clients every 1-2 weeks to enable them to make any changes or refinements promptly.
- The Business Analysts (BA) acts as a primary contact person for a client, having regular Teams/Skype meetings, systematizing all the requirements correctly and showing demos (sprint releases). The BA is also responsible for the conformity of the final product to the documented requirements.
- Communication by email is used when our clients need time to make important strategic decisions.
EHR System Testing Plan
The high quality of a custom healthcare software can be guaranteed only when a proper testing process is established. Our experienced EHR project manager Dmitry Garbar applied best practices to boost the productivity of the EHR software development and testing team on the EHR project.
The system then can be successfully implemented into clinics.
EHR System Architecture
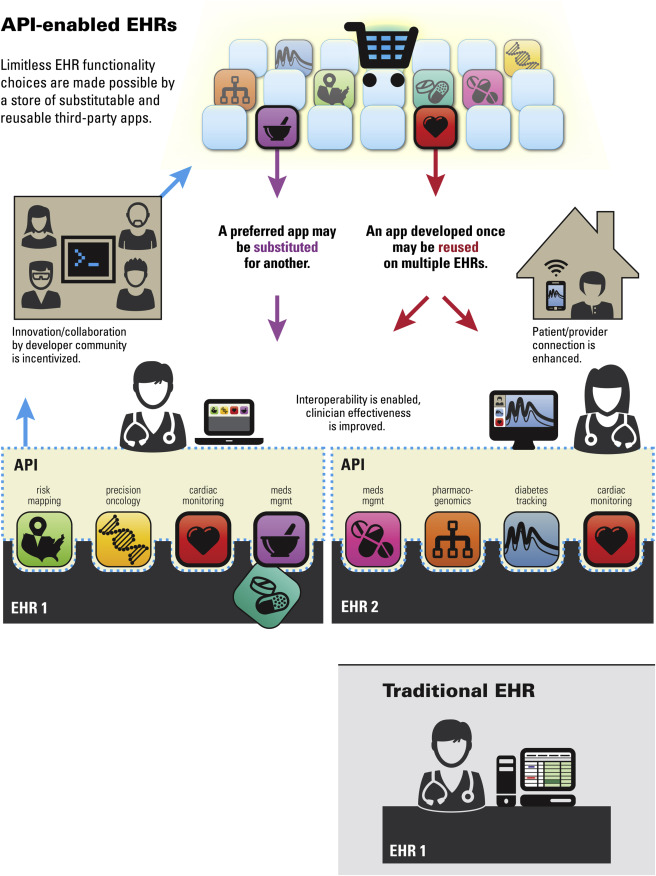
API-enabled EHR
Modern EHR system is a medical database software with user-friendly interface and forms for gathering, accessing, managing and transferring clinical records (also called “health records”, “medical records”, or “patient records”).
According to the U.S. Department of Health and Human Services, the core function of an EHR is integration and access to the storage using interoperability standards (such as HL7 FHIR). In fact, we talk about so-called "API-enabled EHR database".
All eligible professionals and hospitals in the USA are obligated to use CEHRT - 2015 edition certified electronic health record technology - to meet the requirements of the Promoting Interoperability Program (Meaningful Use).
The ability of an interoperable EHR platform to seamlessly integrate with other medical systems and devices along with business intelligence reports generation and clinical decision support can enable medical business excellence.
The project development team uses the interoperability approach to architecture design. The application is often splitted into several modules (services) and these modules communicate with each other and third-party modules via REST API. This type of architecture provides great possibilities of scaling, fault isolation and maintenance. The HIPAA compliant server architecture is proposed by Belitsoft to clients to make sure that the medical application meets the HIPAA's technical requirements.
The architecture of the system often contains the following parts:
1) Backend: Database Layer (for example, MySQL) and API layer (API for the web admin panel and API for the frontend apps);
2) Frontend: tablet-friendly mobile and web application. Tablets are very convenient tools that are widely used in leading hospitals and healthcare systems.
3) Frontend: web admin panel based on React.js or other frameworks of choice for form templates and User Management.
To prevent the loss of patients’ information, we develop a synchronization module. If a doctor’s tablet goes offline while they’re entering clinical data, this module will save the notes and upload them to the cloud when the Internet connection is restored.
However, the arhcitecture of the EHR solution may be significantly more complex that this one like here when cloud technologies are involved.
Core EHR Modules We Often Deal With
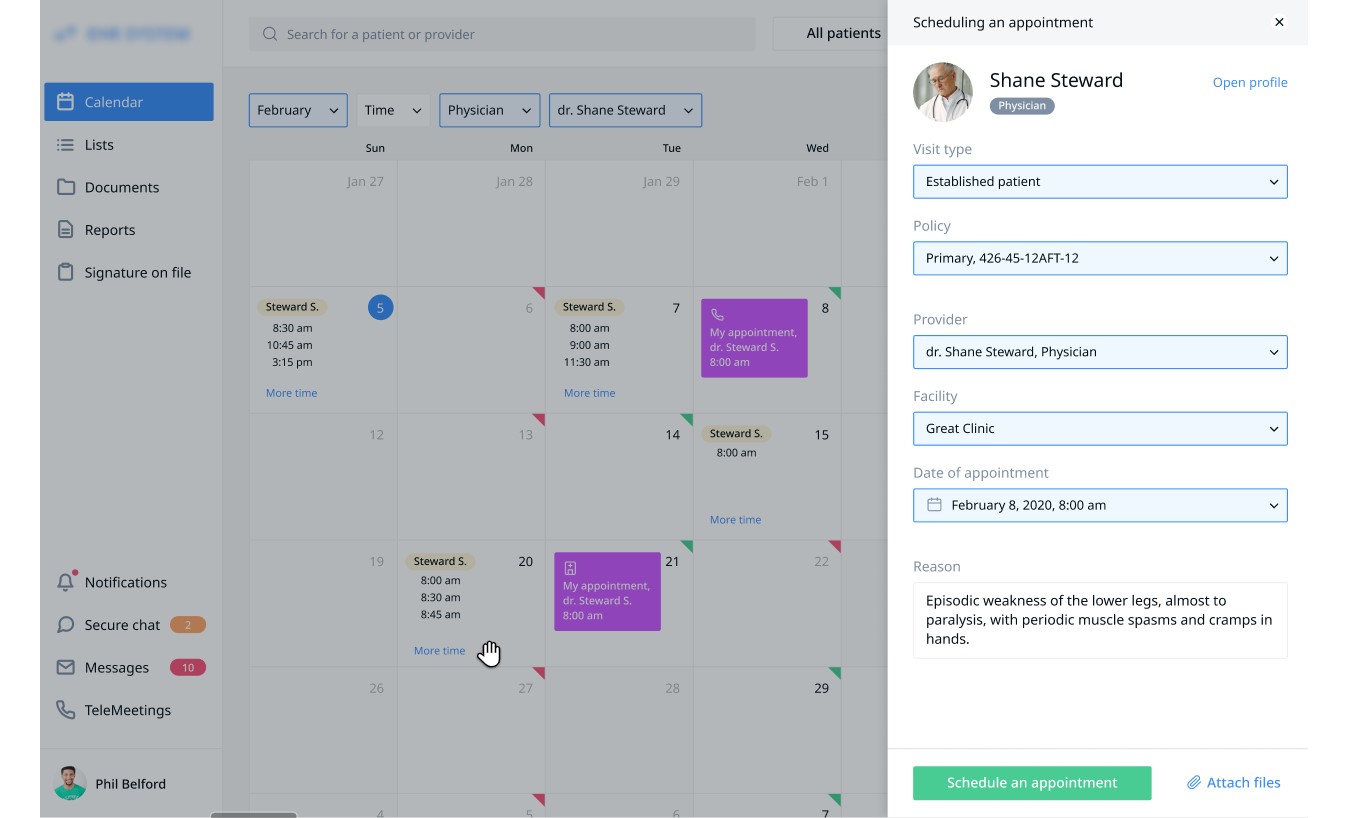
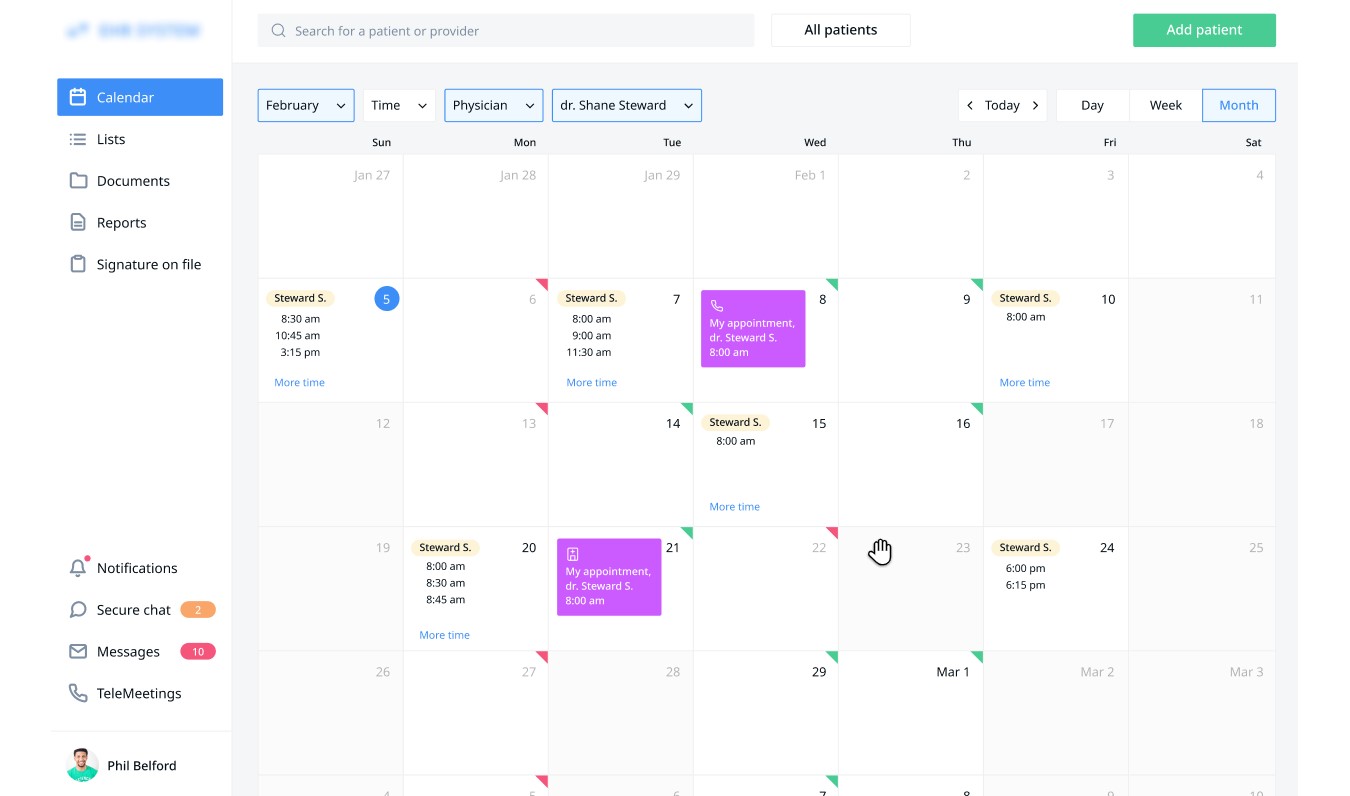
Medical Scheduling Module
A medical scheduling module for EHR system is often integrated with billing and practice management modules.
Below see a use case of a receptionist checking a patient in.
.jpg) Today is February 5. A patient named Shawn Robertson asked to schedule a visit from 5 to 12 of February at any time and with any physician. Theresa Russell, a receptionist, sees that there are several options available during that period. She offers Shawn Robertson to visit Dr. Simon McKinney on February 7 at 8.30 AM.
Today is February 5. A patient named Shawn Robertson asked to schedule a visit from 5 to 12 of February at any time and with any physician. Theresa Russell, a receptionist, sees that there are several options available during that period. She offers Shawn Robertson to visit Dr. Simon McKinney on February 7 at 8.30 AM.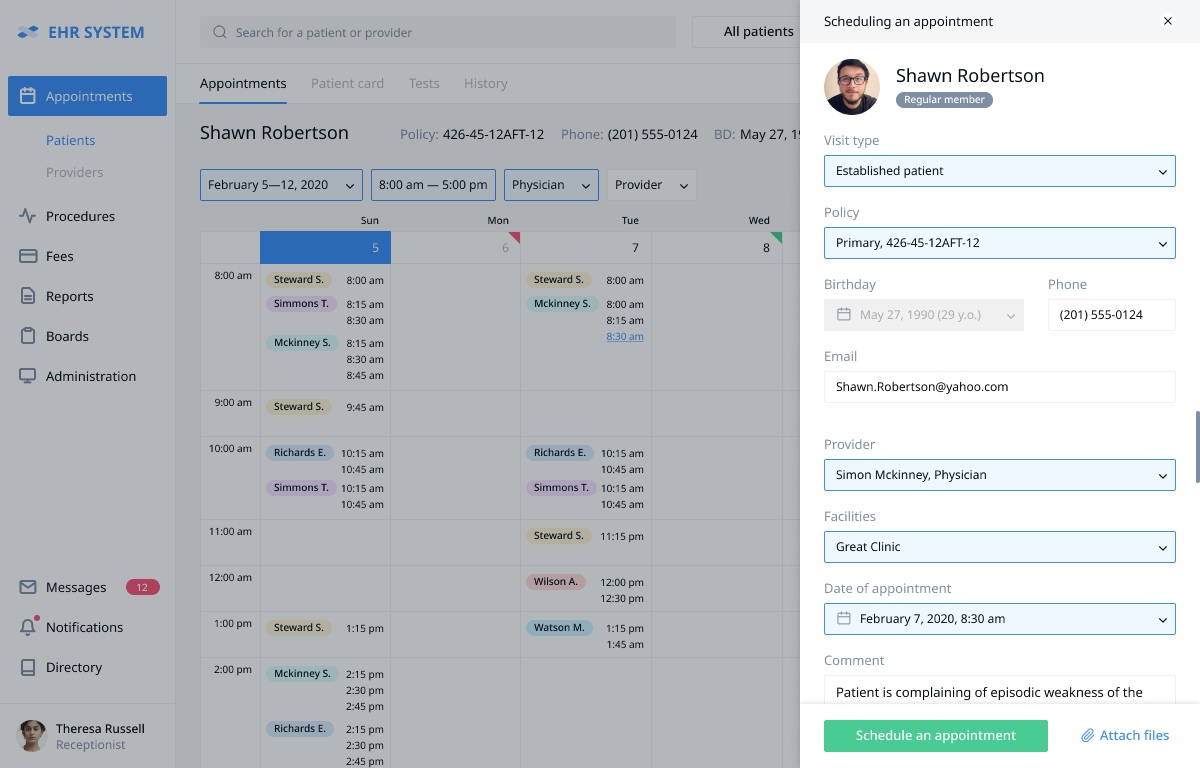 After getting the patient's consent, the receptionist clicks the chosen time slot. A pop-up window appears and offers Theresa to confirm the chosen time slot, the relevant patient data is automatically pulled from the system's database. After clicking the "Schedule an Appointment" button the patient is signed up.
After getting the patient's consent, the receptionist clicks the chosen time slot. A pop-up window appears and offers Theresa to confirm the chosen time slot, the relevant patient data is automatically pulled from the system's database. After clicking the "Schedule an Appointment" button the patient is signed up.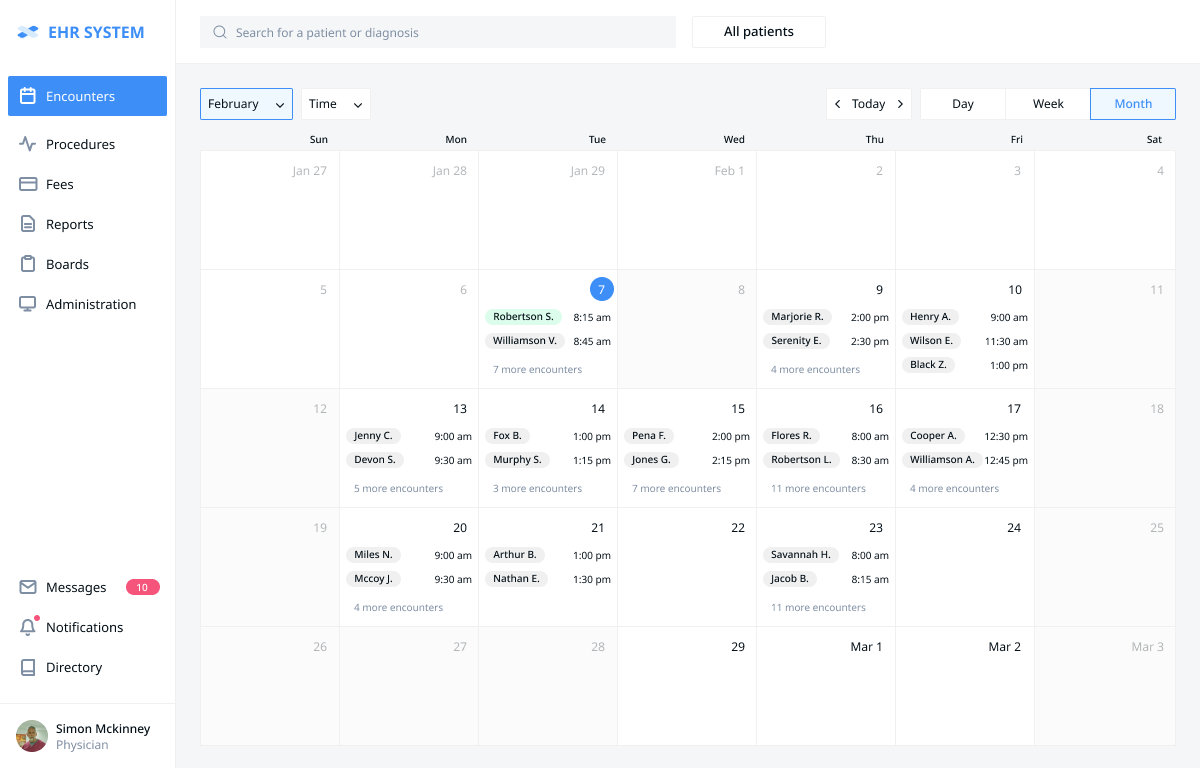 After getting authorized Dr. Simon McKinney moves to the “Encounter” tab and sees the patients that have a visit scheduled during the chosen timeframe (e.g. today, this week, this month). Today, on the 7th of February, there are 9 patients scheduled. The doctor sees the names of the first two and can look up the brief information on all the patients by clicking the “7 more encounters” link.
After getting authorized Dr. Simon McKinney moves to the “Encounter” tab and sees the patients that have a visit scheduled during the chosen timeframe (e.g. today, this week, this month). Today, on the 7th of February, there are 9 patients scheduled. The doctor sees the names of the first two and can look up the brief information on all the patients by clicking the “7 more encounters” link.
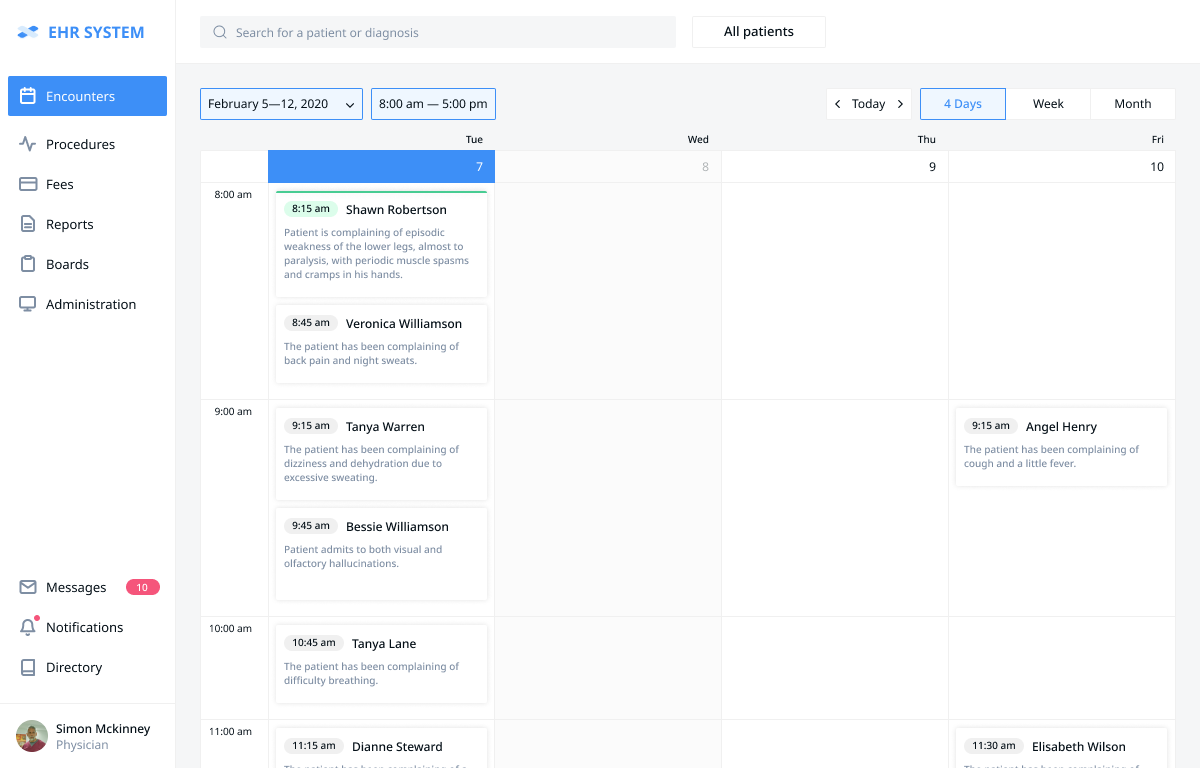 After clicking the “7 more encounters” link Dr. Simon McKinney can see the brief information (including the chief complaint, if mentioned) about each patient to be seen today.
After clicking the “7 more encounters” link Dr. Simon McKinney can see the brief information (including the chief complaint, if mentioned) about each patient to be seen today.
EHR Charting Module
Medical charting is the systematic documentation of interactions with patients concerning a patient's care, condition, and treatment. It is also a legal document: medical providers are required to keep detailed charting documentation, which could affect claims reimbursement in the case of an audit. With custom charting module the provider can spend less time typing, and focus on the patients and their health.
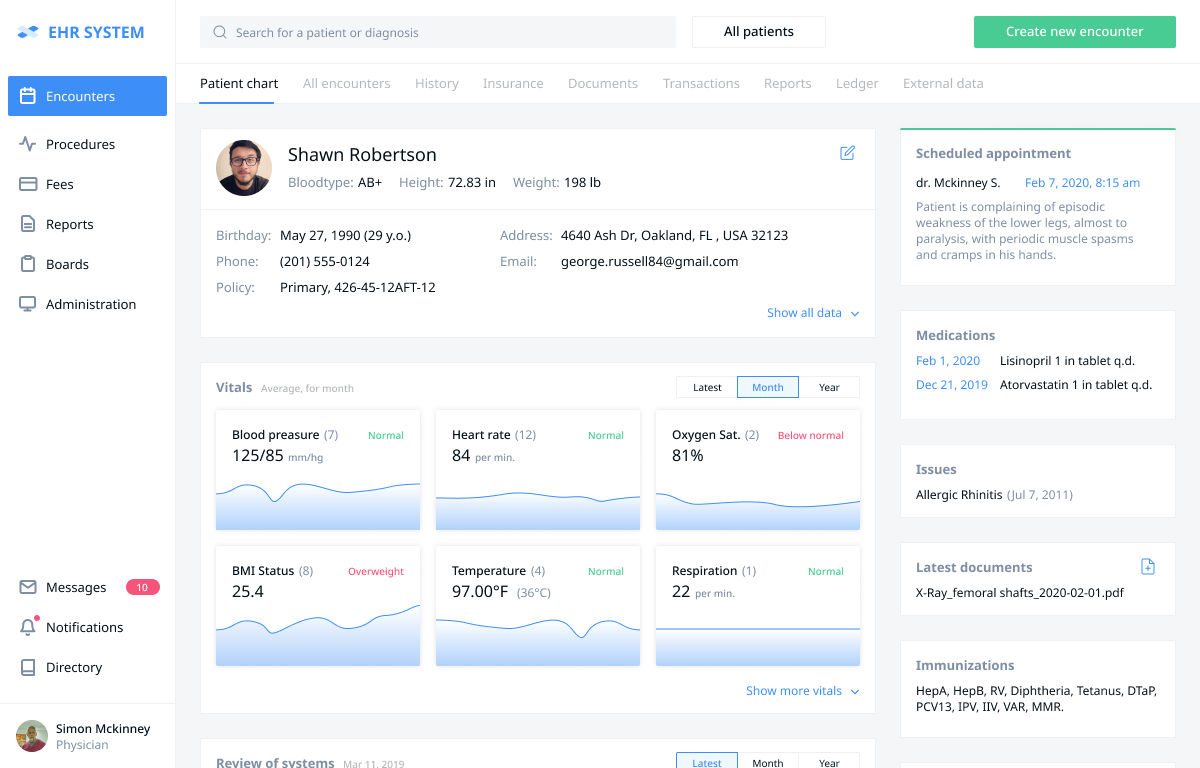 Dr. Simon McKinney clicks the patient’s name and moves to the “Patient Chart” section - a medical dashboard that pulls generalized historical data about the patient from other sections of the system: demographics, vitals, allergies, latest documents (e.g. lab results, a user can add new documents straight from the dashboard without opening additional windows), prescriptions, immunizations, medications. The “vitals” section shows the vital signs’ history and deviations from the norm if any. The information can be filtered by specific timeframes.
Dr. Simon McKinney clicks the patient’s name and moves to the “Patient Chart” section - a medical dashboard that pulls generalized historical data about the patient from other sections of the system: demographics, vitals, allergies, latest documents (e.g. lab results, a user can add new documents straight from the dashboard without opening additional windows), prescriptions, immunizations, medications. The “vitals” section shows the vital signs’ history and deviations from the norm if any. The information can be filtered by specific timeframes.
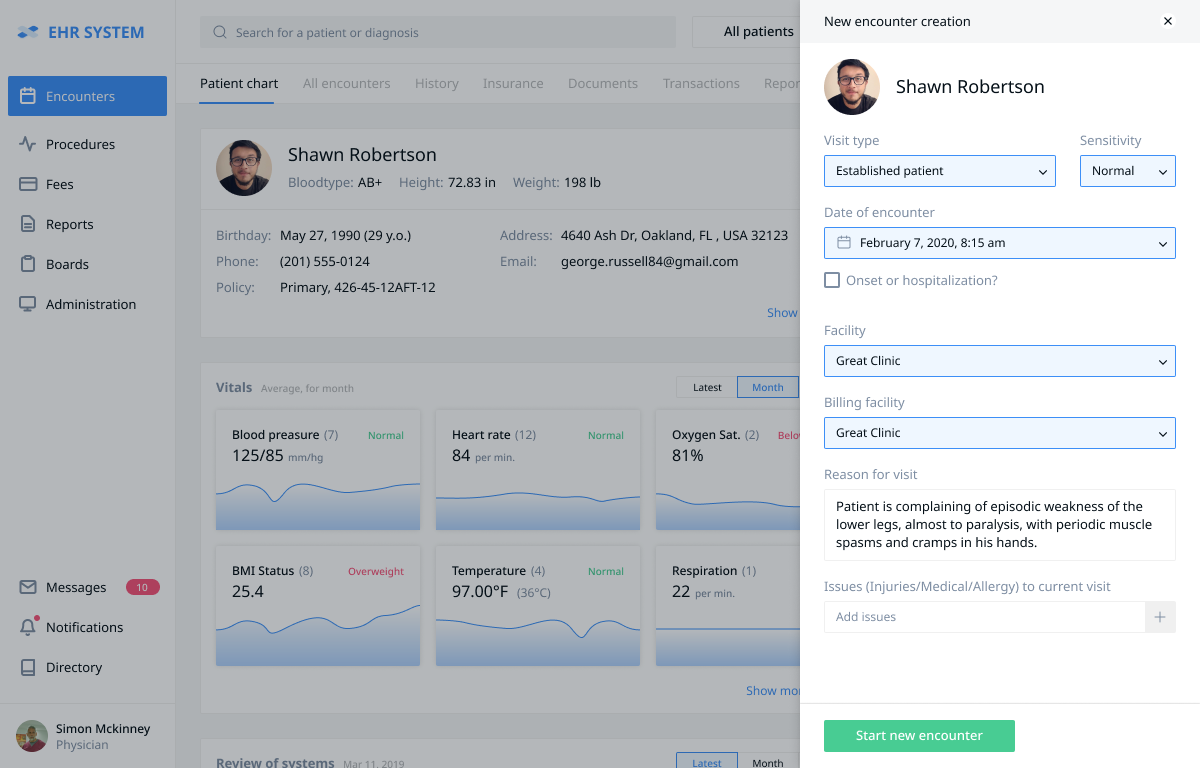 At the beginning of the encounter, after pressing the “create new encounter” button, a pop-up window appears that automatically pulls patient information necessary to begin the encounter. Dr. Simon McKinney can enter the chief complaint if it wasn’t entered earlier. They can also add the patient’s general information, if necessary.
At the beginning of the encounter, after pressing the “create new encounter” button, a pop-up window appears that automatically pulls patient information necessary to begin the encounter. Dr. Simon McKinney can enter the chief complaint if it wasn’t entered earlier. They can also add the patient’s general information, if necessary.
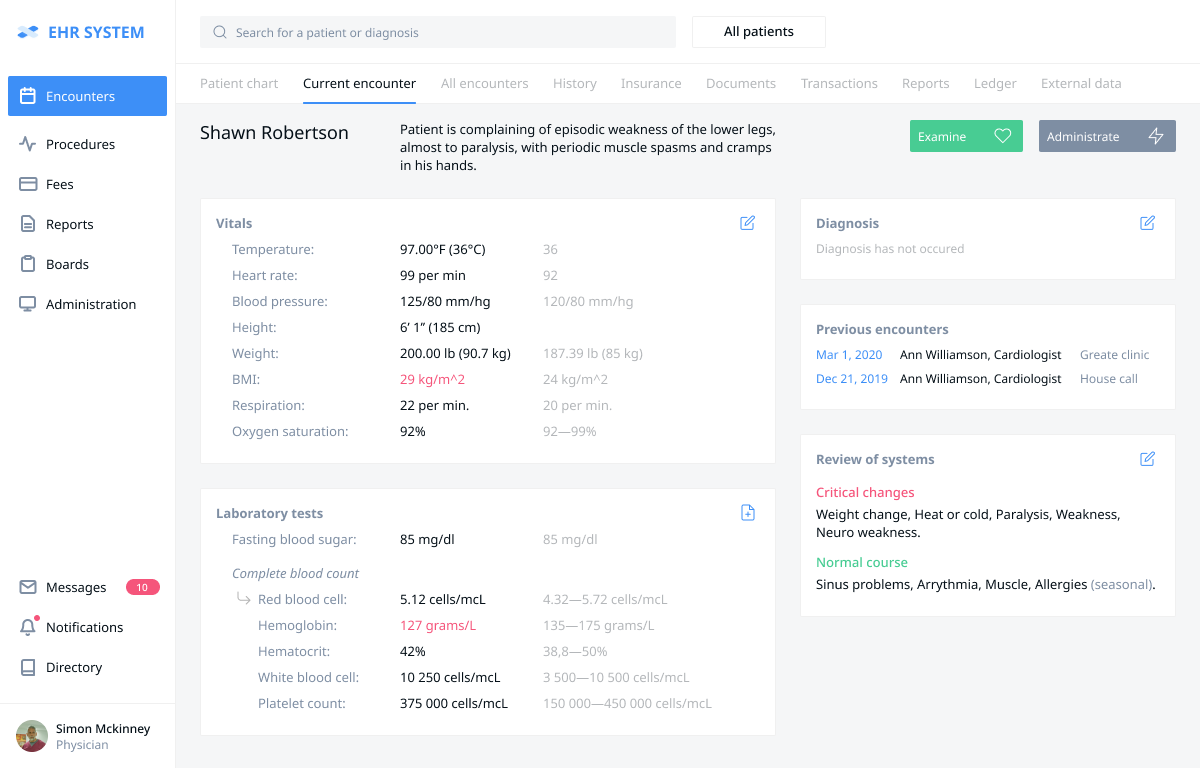 After pressing the “Start new encounter” button Dr. Simon McKinney goes to the empty form of the current encounter (this slide shows the finished visit with the conducted examinations). To begin the diagnostic process, the doctor presses the “Examinations” button. To begin the billing process, the doctor (or the receptionist) presses the “Administration” button.
After pressing the “Start new encounter” button Dr. Simon McKinney goes to the empty form of the current encounter (this slide shows the finished visit with the conducted examinations). To begin the diagnostic process, the doctor presses the “Examinations” button. To begin the billing process, the doctor (or the receptionist) presses the “Administration” button.
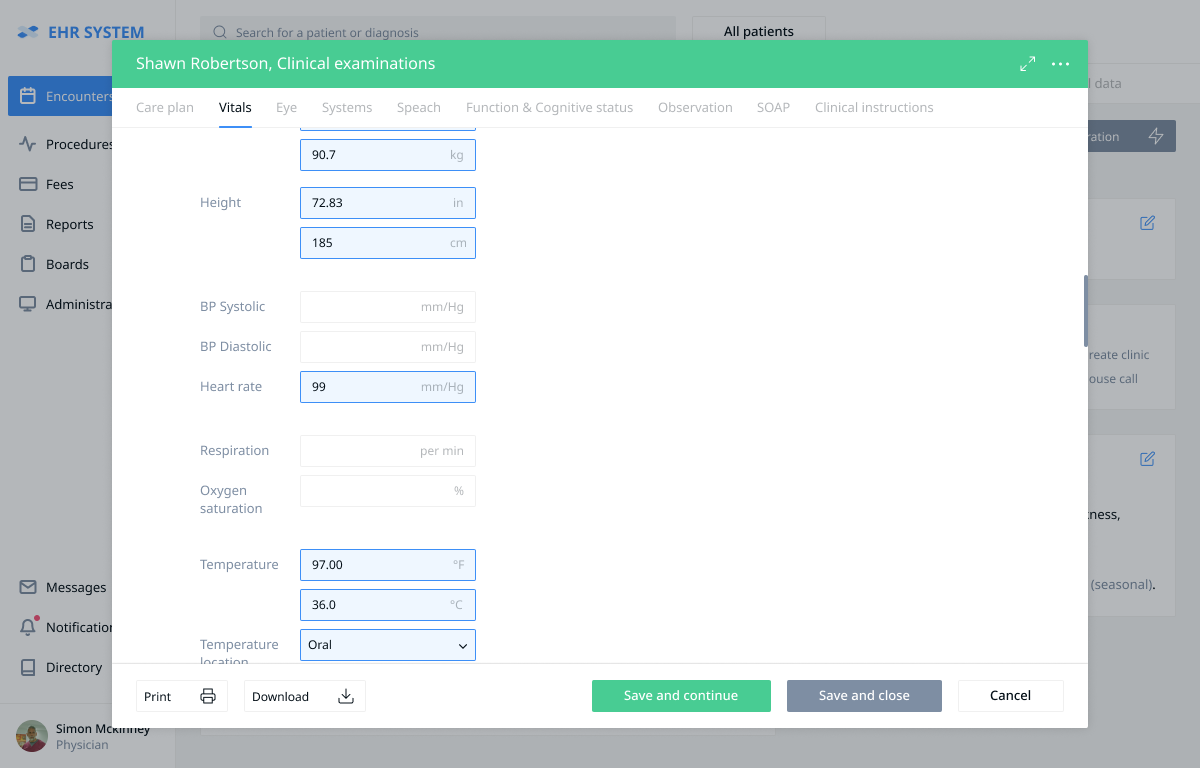 After pressing the “Examinations” button a pop-up window containing the available examinations appears. A user can select the necessary examination by pressing the appropriate tab at the top of the page.
At this stage, the doctor fills in the vitals and can either save and close the examinations panel or save and continue with the examinations.
After pressing the “Examinations” button a pop-up window containing the available examinations appears. A user can select the necessary examination by pressing the appropriate tab at the top of the page.
At this stage, the doctor fills in the vitals and can either save and close the examinations panel or save and continue with the examinations.
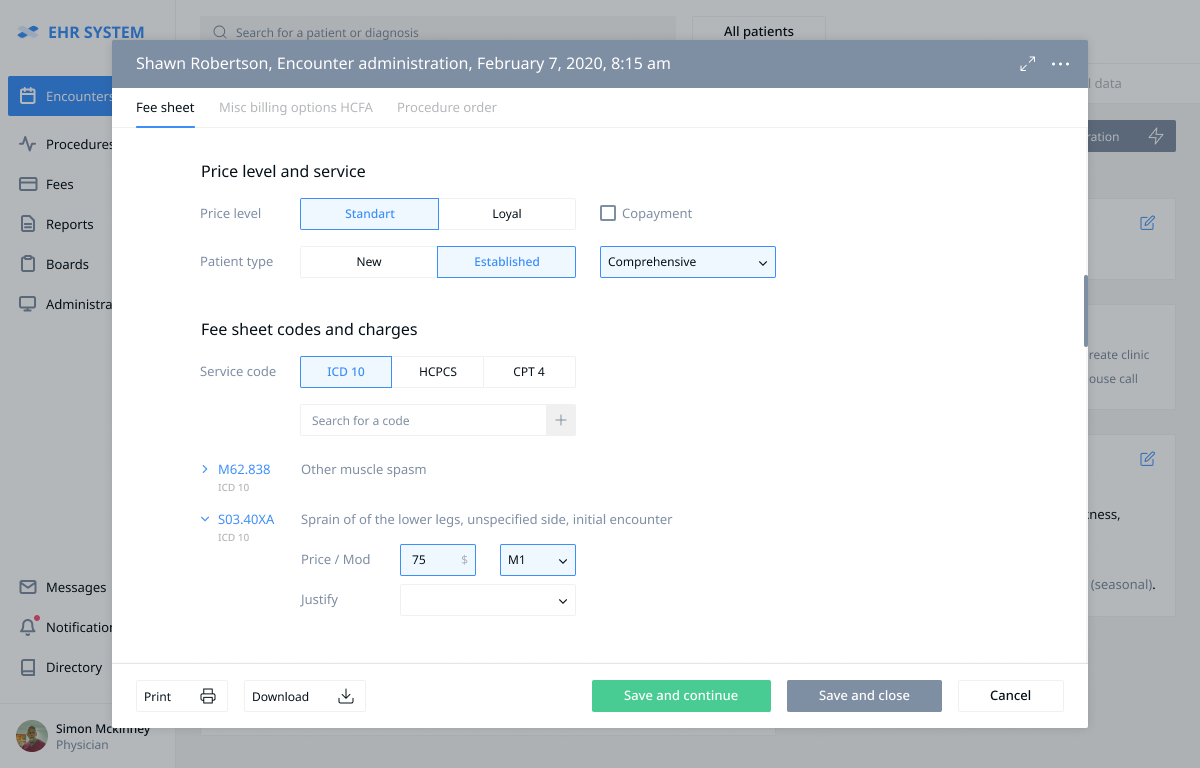 The doctor presses the “Administration” button causing a pop-up window to appear. This window shows the available options to begin the billing procedure. The “Fee sheet” section allows the doctor to choose the price level and patient type. Then the doctor chooses the codes of the conducted procedures according to CPT4, as well as the ICD-10 diagnosis (the doctor can enter a keyword or part of the code into the search window to quickly choose the necessary code from the list). The chosen codes are displayed below, possibly with the prices and modifiers. The diagnosis should be supported by a procedure in the “Justify” field. After the billing form creation is complete the doctor presses the “Save and close” button and finishes the encounter.
The doctor presses the “Administration” button causing a pop-up window to appear. This window shows the available options to begin the billing procedure. The “Fee sheet” section allows the doctor to choose the price level and patient type. Then the doctor chooses the codes of the conducted procedures according to CPT4, as well as the ICD-10 diagnosis (the doctor can enter a keyword or part of the code into the search window to quickly choose the necessary code from the list). The chosen codes are displayed below, possibly with the prices and modifiers. The diagnosis should be supported by a procedure in the “Justify” field. After the billing form creation is complete the doctor presses the “Save and close” button and finishes the encounter.
Medical History. This element logs the patient’s conditions throughout their life. It can include the growth chart, medication and immunization history, allergies, family and social data, habits (e.g. smoking and alcohol use), surgeries, obstetric information and more. Having it on hand allows doctors to gain insights as to the causes of the patient’s current condition.
Medical Encounters. When someone visits a physician, this is where the doctor puts the gathered information on the patient’s current condition. Encounter data includes the chief complaint, history of present illness, physical examination results, vital signs, assessment, and treatment plan.
Orders and Prescriptions. This feature creates and stores the medication orders and prescriptions. These can be printed or sent electronically to the pharmacy straight from the point of care. Capabilities: submit e-prescriptions from your patient’s chart, automatic drug-drug and drug-allergy interaction checks, send prescriptions electronically to your patient’s local pharmacy, complete prescription refill requests electronically, view prescription costs at various pharmacies and medication alternatives, medical decision support, e-prescribing of controlled substances.
Progress Notes. Regular, chronological updates on the patient’s condition. These are used mostly for hospitalized patients and can be entered by all clinical professionals participating in the care: doctors, nurses, pharmacists, dentists, etc.
Test Results. Blood tests, biopsies, X-rays and other similar examinations are stored and managed by this module. Images (e.g. MRIs) can be either stored as-is using formats like DICOM or handled elsewhere, in which case the chart will likely contain the reports as text.
Information exchange. To increase their efficiency, the charts should exchange data with other modules in your EHR/EMR. Demographic information and vital signs (heart rate, blood pressure, temperature, etc.) should automatically be taken from other modules and entered in the forms so that the clinicians don’t have to do it several times. And integration with the billing module can help with assigning codes and decrease the number of errors.
PHI Copying. According to HIPAA, patients can ask for and receive a copy of their personal health information (with certain caveats). This means that the charts should be either printable or convertible to a popular electronic format, e.g. PDF.
Guidelines. Including information like normative lab values, weight parameters, dosage guidelines, screening recommendations, etc. gives the physicians a benchmark to quickly measure patient stats against. A reference point like this helps doctors provide better care. These values can also be accessible to the patients via the portal, thus improving their knowledge about their own health.
Customizable/Specialty-specific Charting Templates. A dentist and a psychiatrist can include different things in the patient charts. So it would be preferable if the system adapted to accommodate their needs. This could be either done by making the charts highly customizable or including specialty-specific templates in the charting module.
Speech-to-text. Dictating notes instead of typing them allows doctors to spend more time with the patient instead of the computer. The physician’s spoken words can either be transferred straight to the EHR/EMR and reviewed by the same physician later, or they can be sent to a medical scribe for a preliminary check first.
EHR Telemedicine Module
E-visits and medical consultations. The main idea of telehealth is to connect patients and physicians around the world quickly and securely through live video. This enables two-way, face-to-face interactions on a computer or mobile device with high-quality video and audio.
Secured communication can be held by a wired or wireless Internet connection.
The solution also allow screen sharing and multiway video so 3rd parties (such as caregivers or translators) can participate in a virtual consultation. All the additional attendees are added by the doctor.
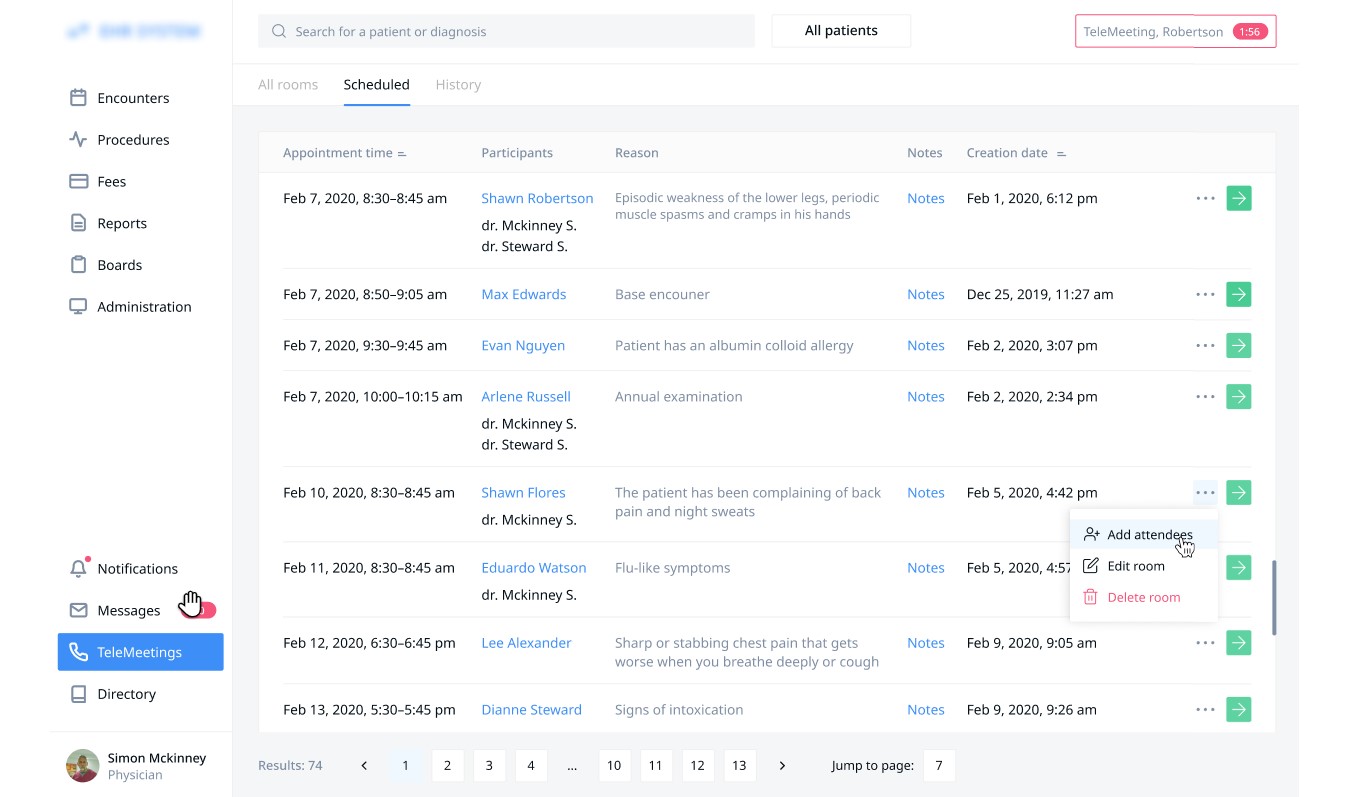
Consultation Notes. The feature allows doctors to create notes during the sessions with patients in order not to lose goals, medications prescribed, invoices, follow up appointments, or care plans they may have discussed.
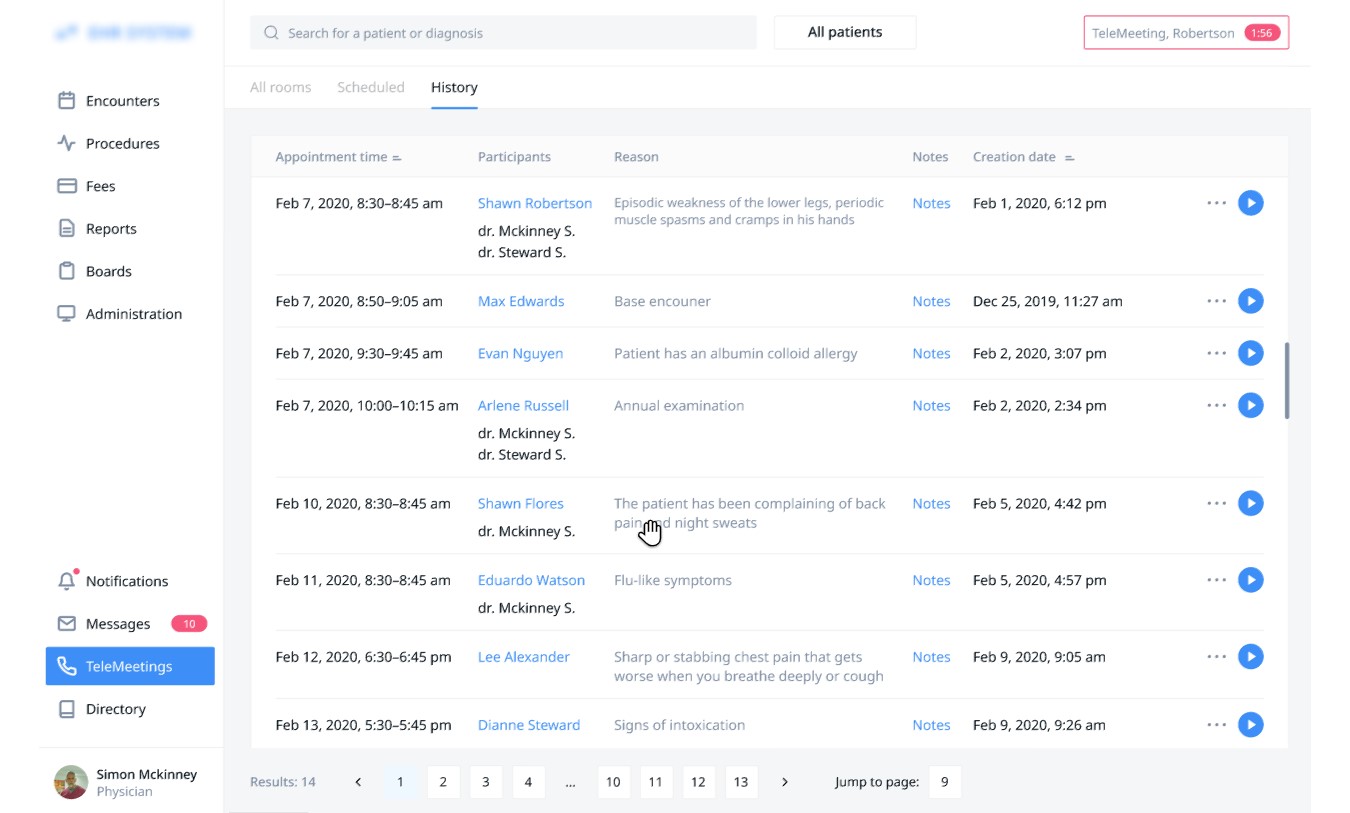
Patient-initiated. Patients can book follow-up appointments to their clinic visits or online consultations and consult with you via video sessions. This will definitely save the providers’ time compared with written communication.
Moreover, the patients can clearly see the type of appointment while checking their schedule so that they can plan their visits or video calls.
EHR Voice Recognition
Doctors and nurses were spending too much time on EHR-related tasks. This meant they either had less time for patients or more overtime work. Implementing speech recognition could be a solution to the problem - by talking to the machine the medical professionals could enter information quicker and even do it while examining the patient.
The speech recognition system integrated with our client’s EHR was built as an on-premise solution due to security concerns.
Its most notable features included:
- Voice input of text and numbers;
- Voice commands for navigation inside the system;
- Automatic expansion of medical acronyms and abbreviations;
- An option of adding more dictionaries for medical specializations;
- An option to adapt to the voice of a specific medical professional.
The first release included three core dictionaries: general medicine, pathology, CT/MRT.
Each contained the data the system needs to recognize and process the words relevant to the appropriate niche. The “general medicine” dictionary was useful for all fields within medicine, while “pathology” and “CT/MRT” had relatively few words and were cost-effective to implement. The system also included the option to expand the dictionary list, as mentioned above.
As one of the customer’s requirements we have also created an open API for the system to make it easy to integrate with other medical solutions.
We have also been tasked with finding the most suitable headset for doctors and nurses. It had to be convenient enough to be worn 8 hours a day and provide high signal quality.
The resulted system has successfully solved the customer’s problems.
Time spent on clerical tasks has decreased by 23%. The results were even better with older doctors, who were experts in medicine, but not experts in computers. Moreover, the focus group has reported higher satisfaction with their work environment.
Patient Portal Features
Medical patient portal is an extension of EHR. Data from it is published by a healthcare organization to the application with 24/7 online access.
Accessing personal health information. Having entered a unique username and password, patients can browse (and print if necessary) health information including recent doctor visits; case reports; medication lists; immunizations; allergies; lab & test results.
Updating contact and demographic information. Get patients to complete their registration and update their information online. Health professionals, for their part, have to check the accuracy and quality of registering data before it is accepted into their EHR.
Scheduling appointments online. Patients can get the appointment booked via the portal without going through the hospital telephone system and auto attendants. They receive an alert as the doctor confirms or reschedules the appointment.
They later modified the feature, making patients able to request a viable appointment. Thus, they can browse the hours for each location, every doctor who works there and their timetable, as well as check-up types they accept.
Patient portals can help practitioners with cutting down on phone calls and decreasing non-appearance.
Messaging with a healthcare team. When a patient portal is integrated with an EHR system, secure encrypted messaging is the simplest and most efficient way to exchange information and test results both for patients and medical professionals.
Receiving notifications. If a patient books an appointment with a health professional, the system can reply with an e-mail, a text message (SMS) or a push notification to a mobile device. Plus, users can be reminded to take prescription medication or check a glucose level if the patient has diabetes.
Integration with third-party apps and systems. More and more people use monitoring devices. Whether it be a fitness tracker, a medication reminder or a glucose monitor, these systems store patient vitals and can be useful for diagnosis and treatment.
To reduce the amount of data entry required, patients can upload information directly from medical devices, fitness trackers or smartphones.
Payments. Patient portals enhance customer experience in many ways, especially when providing the ability to make payments. This option makes it easier for patients to understand and handle their financial responsibility.
So, what payment features should be supported?
- Insurance information: Login to the portal and view/update insurance data.
- Billing query: Submit billing-related questions via the patient portal.
- e-Payment: Make online payments via multiple modes.
- History storage: View records of medical payment amounts and dates in one place.
- Saved payment method: Securely hold a credit card or bank information for repeat payments.
Downloading and completing registration forms. Whether patients complete registration forms online or when they are in the office, it usually takes 10 to 15 minutes to do all the paperwork. For those who complete pre-visit forms online, the system has to notify them of how long it takes to register.
Accessing educational materials and communities. Just as patients want to see their health history, they also want to figure out these records. However, diagnoses and treatment plans are usually difficult for users to understand. With a portal, they are able to access supplemental information online.
For users with lower health literacy, some health IT providers integrate natural language processing to translate certain clinical terms, thus making patient portal records more accessible.
The most effective way to improve customer health literacy lies in offering patient education where applicable. More and more health IT vendors have signed licensing agreements with educational platforms, allowing them to integrate patient education materials into their systems.
Patients often seek out people with similar health states for advice and support. Thus, for example, our client asked us to create a website for a community of people challenged with different diseases. Having logged in, they can access blog posts, chat with other community members and express their emotions with special icons.
Medical Billing Module
EHR needs to have a robust module to handle payments and reimbursements. Capabilities: generate invoices for the consultation and procedures, tracking payment status, automated billing codes transcription, composing and submitting claims to the insurance agencies, track the status of the claims (received, accepted for processing, denied or rejected), alerting on rejected claims with clarification, E/M Calculator, insurance card scanning, copayment calculator, automated eligibility verification.
Claim Submission. This feature allows the practice to create superbills and electronically submit claims to a clearinghouse or directly to the insurance company. It must also be able to generate bills and patient statements for the patients who need to pay for the visit.
The claims are usually submitted in groups to save staff time. However, if even one of the claims is found to be non-compliant with HIPAA, the whole batch will be sent back for corrections, which cost time and, therefore, money. That is why EHR providers integrate “claim scrubbing” - automatic checking for errors before the claim is submitted.
It is estimated that 90% of claim denials are preventable by using better procedures, making a well-designed submission module a valuable tool for improving a practice’s bottom line.
Copayment/Coinsurance/Deductible Processing. Your EHR should notify the reception staff if a patient needs to pay for the visit out of their pocket. This would help your practice increase the collection rate. Given the abysmal overall payment rates among patients (e.g. the average payment rate for people with high-deductible plans receiving outpatient care is only 18.2%), any improvement in this area is bound to be meaningful.
Billing Reports. You can’t manage what you can’t measure, which is why EHR needs flexible billing reports. They will demonstrate the rates of reimbursement and patient collections, recent and historical trends, and more.
Many off-the-shelf EHRs have the option to create custom reports or tailor the existing ones to better fit the needs of the practice. In turnkey systems, the nature and flexibility of the reports are discussed in advance and then created according to the customer’s requirements.
Claim Rejection Analysis. This module processes the rejected claims and highlights the errors that need to be corrected. The reasons could include incomplete or incorrect information, non-covered services, missing codes, etc. When the mistakes are fixed, the claims can be resubmitted.
Automated Coding. ICD-10 has almost 70.000 diagnosis codes. Together with a multitude of CPT codes, this creates a problem for the billing staff, as coding mistakes can lead to claim rejections or denials. An automated system will help the clinicians with assigning the correct values to the diagnosis and treatment, and will also transfer these values to the claim form, reducing human involvement and risk of error.
A specialty-specific EHR, e.g. for Orthopedics or Behavioral Health, might have a module that suggests the codes most relevant for that specialty. This makes the work of clinicians and coders easier and once again decreases errors.
Automated Eligibility Verification. The EHR can be integrated with the insurance companies’ databases. As a result, the administrative staff can see the patient’s insurance details (if the patient is covered), and the clinic can avoid rejections.
Moreover, this data can also be transferred directly to the claim form to save time and decrease risk.
Payment Tracking. This module helps manage financial resources by following each bill through every stage of its processing, from submission to payment. With this information, the administrative staff can estimate the reimbursement timeline
Integrated Clearinghouse. A clearinghouse is a system that processes the documents sent from medical practice to the insurance company and vice versa (claims, 835 forms, etc.). Its purpose is to convert the data to the format that the receiving company’s software would accept.
It is often a third-party solution. However, there are EHRs that have a built-in clearinghouse, thus eliminating the need for intermediaries and saving the practice money on using external services.
Messaging. An inbuilt messaging system will allow quick and secure communication between clinicians and administrative staff, which would be useful in claims preparation and rejection analysis. The same feature could be reused in a patient portal or for coordinated patient care if your EHR is connected to those of your partners - labs, specialized medical centers, etc.
Referral Management. In certain cases, if the incoming patient doesn’t have a referral the insurance might not pay for their treatment. Having an integrated referral management system will help your billing team and reception employees be aware of the situation. Moreover, it will automatically inform the referring practice about the visit, closing the loop and freeing your employees from the need to follow-up via phone or fax.
Accounts Receivable Management. If a claim has been denied it doesn’t mean that your practice will never see that money. More than three-quarters of them are eventually paid. But your employees need to work to make it happen. That’s where an A/R management system will come in handy. It tracks the outstanding payments, helps correct the forms and resubmits the claims.
Lab Integration Module
Capabilities: submit patient lab orders directly from chart; receive patient test results; share results with patients via the patient portal; automated reporting and analysis of the results (notification if normal parameters are overcome); submit electronic data on reportable lab results to public health agencies; checking lab results for possible impact of prescribed medication.
Appointment Management for Patients and Staff
Capabilities: scheduling an appointment via Patient Portal, website or manually by practice's personnel; automated check-in for physicians availability and preventing double bookings; appointment reminders via phone call, SMS, email and other means; patient recall system; appointment calendar with color coding; forming of wait lists of patients; automated notifications for cancelled appointments; calendars synchronization (iCal, Google or Outlook); composing schedules for clinicians (setting available dates & times, time-breaks, and locations); appointment management for receptionists (comparing physicians’ strains, view physicians’ appointments per day, week or month, schedule a recall visit); flowboard (filter by date, visit category, visit status, facility, physician).
Send us your request for information to learn more. We can customize EHRs and improve UI/UX Design; develop additional functionality; help you deploy it to the cloud; set up backups; transfer data from your old EHR; provide you with dedicated technical support; consult you during your EHR implementation.
Rate this article
Recommended posts
Portfolio

Our Clients' Feedback
















.jpg)
.jpg)
.jpg)
.jpg)
.jpg)
.jpg)
.jpg)
.jpg)
.jpg)
.jpg)
.jpg)
.jpg)
.jpg)
.jpg)
.jpg)
.jpg)
.jpg)
.jpg)
.jpg)
.jpg)
.jpg)
.jpg)
.jpg)
.jpg)
.jpg)
.jpg)
.jpg)
.jpg)
.jpg)
.jpg)
.jpg)
.jpg)
.jpg)
.jpg)
.png)
.png)
.jpg)
.jpg)
![How to Create a Language Learning App [The Ultimate Guide!]](/uploads/images/blog/posts/previews/image_155352483594-image(600x250-crop).png)
.jpg)
.jpg)
.png)
.jpg)
.jpg)
.jpg)
.jpg)
.jpg)
.png)
.jpg)
.jpg)
.jpg)
.jpg)
.png)
.jpg)
.jpg)
.jpg)
.jpg)
.jpg)
.jpg)
.jpg)
.jpg)
.jpg)
.jpg)
.jpg)
.jpg)
.jpg)
.png)
.jpg)

















We have been working for over 10 years and they have become our long-term technology partner. Any software development, programming, or design needs we have had, Belitsoft company has always been able to handle this for us.
Founder from ZensAI (Microsoft)/ formerly Elearningforce